The latest bit of good news for the programmed death receptor-1 (PD-1)–targeting antibodies in advanced melanoma comes for pembrolizumab (MK-3475). While the results came from only a phase I study, they were among those chosen for presentation at an ASCO press briefing during the Annual Meeting.
“We were excited to see that pembrolizumab was effective in previously untreated patients as well as in those who had multiple prior therapies, including ipilimumab (Yervoy). These are early data, but they tell us we are onto something really important,” said Antoni Ribas, MD, PhD, Professor of Medicine at the David Geffen School of Medicine at the University of California, Los Angeles.
Steven O’Day, MD, Director, Clinical Research, Beverly Hills Cancer Center, Beverly Hills, California, who moderated the press briefing on progress in immunotherapy, commented, “The remarkable thing is that almost 90% of the patients that respond are having durable responses with a toxicity profile that is almost unheard of in metastatic cancer. This is really extraordinary about this class of drugs.”
Pembrolizumab is an antibody designed to block the interaction of PD-1 on T cells and reactivate antitumor immunity. In April 2013, the U.S. Food and Drug Administration (FDA) had previously granted a Breakthrough Therapy designation to pembrolizumab (previously known as lambrolizumab) for advanced melanoma. In May 2014, the FDA granted pembrolizumab a Priority Review designation under its Accelerated Approval program.
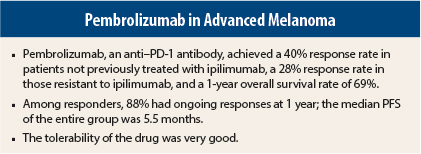
In the KEYNOTE-001 trial involving 411 patients with advanced melanoma, pembrolizumab produced responses in 34% of patients, including 28% of patients whose disease had progressed on prior treatment with ipilimumab. At 1 year, 88% of responders were continuing to respond to treatment, Dr. Ribas reported at the Annual Meeting.
Durable Responses
The study, which is the largest phase I clinical trial ever conducted in metastatic melanoma, included seven different expansion cohorts, some previously treated and some treatment-naive, who received three different dosing regimens of single-agent pembrolizumab. More than half the patients had M1c disease. Chemotherapy had been received by 22% of the ipilimumab-naive arm and 47% of the ipilimumab-pretreated arm; 23% and 30%, respectively, had been treated with other immunotherapies.
By independent review, 34% of patients responded, including 40% of the 190 patients not previously treated with ipilimumab and 28% of the 221 patients whose disease had progressed on prior ipilimumab. “The durability of response is exciting. This is a remarkably high response rate for an antibody that hits the immune system and not the tumor directly,” Dr. Ribas indicated.
At the time of analysis (October 2013), 88% of reported responses were ongoing, and median duration of response had not been reached. The longest response so far has been 76 weeks. The maximum percent change from baseline in tumor size was 72%. No one dosing regimen seemed superior to others, he said.
At 6 months, 45% of patients had not progressed; median progression-free survival was 5.5 months. The estimated overall survival rate at 1 year was 69% (74% in ipilimumab-naive and 65% in ipilimumab-exposed patients), and at 18 months was 62%. Median overall survival was not reached at the time of analysis, Dr. Ribas reported.
Activity was observed across all dose levels and patient subgroups, irrespective of prior ipilimumab therapy, performance status, lactate dehydrogenase levels, BRAF mutation status, tumor stage, and number and type of prior therapies.
Relatively Benign Therapy
“This is one of the most benign therapies I’ve ever used in my clinic,” Dr. Ribas said at the press briefing.
The most common adverse events of any grade were fatigue, pruritus, and rash, but grade 3/4 side effects (these and other toxicities) were limited to 2% or fewer patients and only 12% overall had a grade 3/4 adverse event. Only 4% of patients discontinued treatment due to a drug-related side effect. Safety profiles were similar for ipilimumab-naive and previously treated patients.
Immune-mediated adverse events are especially of interest with this class of agents, and again, the safety profile was very good, he said.
The only such side effects that occurred in more than 1% of patients were hypothyroidism (8%) and pneumonitis (3%); these were grade 3/4 in only one or two patients receiving this drug.
Ongoing randomized controlled studies are further evaluating pembrolizumab in advanced melanoma patients, both previously treated and not previously treated with ipilimumab. Studies in an adjuvant setting are planned. n
Disclosure: This research was supported by Merck. Dr. Ribas reported a consultant or advisory role with Amgen, Compugen, GlaxoSmithKline, Genentech, Merck, Novartis, and Pierre Fabre, stock ownership with Kite Pharma and Flexus Bio, and holds a position as an advisory board member and/or consultant for Merck. Drs. O’Day and Weber reported no potential conflicts of interest. ■
Reference
1. Ribas A, Hodi FS, Kefford R et al. Efficacy and safety of the anti-PD-1 monoclonal antibody MK-3475 in 411 patients with melanoma. ASCO Annual Meeting. Abstract LBA9000. Presented June 2, 2014.