Two hormonal therapies combined are more efficacious than one when used as first-line treatment for hormone receptor–positive metastatic breast cancer in postmenopausal women, finds Southwest Oncology Group trial S0226.
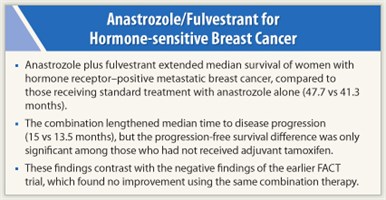
Results of the phase III trial, reported at the 2011 CTRC-AACR San Antonio Breast Cancer Symposium,1 showed that progression-free and overall survival among the 694 patients studied were 1.5 and 6.4 months longer, respectively, for those randomly assigned to anastrozole (Arimidex) plus fulvestrant (Faslodex) than for those given anastrozole alone.
 However, unplanned subgroup analyses suggested that these benefits were largely restricted to women who had not received adjuvant tamoxifen, according to first author Rita S. Mehta, MD, of the University of California, Irvine Medical Center.
However, unplanned subgroup analyses suggested that these benefits were largely restricted to women who had not received adjuvant tamoxifen, according to first author Rita S. Mehta, MD, of the University of California, Irvine Medical Center.
The positive findings of the trial overall are noteworthy in that they contrast with the negative findings of the FACT trial, a smaller trial where 32% of patients were ineligible, which tested the same combination and found no improvement in either outcome.2
“We think our patient population was a more endocrine-sensitive population,” Dr. Mehta speculated. Also, “our trial was not confounded by patients crossing over to combination therapy because patients only crossed over to fulvestrant.”
Differing Patient Populations

 Kathy Pritchard, MD, of the NCIC Clinical Trials Group and the University of Toronto noted that the group had canceled a planned adjuvant trial of the combination based on the earlier negative trial. “Do you think there is enough evidence here [in S0226]—that it’s clear enough that this relates to previous nontreatment with endocrine therapy—that you might suggest this combination should still be taken into the adjuvant setting?” she asked.
Kathy Pritchard, MD, of the NCIC Clinical Trials Group and the University of Toronto noted that the group had canceled a planned adjuvant trial of the combination based on the earlier negative trial. “Do you think there is enough evidence here [in S0226]—that it’s clear enough that this relates to previous nontreatment with endocrine therapy—that you might suggest this combination should still be taken into the adjuvant setting?” she asked.
“It’s actually [due to] multiple factors. We think that it’s probably that this was a relatively nontreated patient population…, [and] we think we may have picked out an endocrine-sensitive population,” Dr. Mehta replied, which would indeed make the findings applicable to the adjuvant population.
Discussant James N. Ingle, MD, of the Mayo Clinic in Rochester, Minnesota, agreed that differing patient populations between trials may have played some role. He warned against putting too much emphasis on a negative unplanned subgroup analysis in an otherwise positive trial.
“The unplanned subset analysis finding of no benefit in prior tamoxifen patients should be interpreted with caution,” he maintained. “If confirmed, it would suggest that the combination is of value only in endocrine therapy–naive women with metastatic disease. These are uncommon today, and the only place you could probably find these women is in the adjuvant or neoadjuvant setting.”
In sum, Dr. Ingle said, the field now has two randomized trials with conflicting findings. “The combination of anastrozole plus fulvestrant cannot be recommended as a new standard in women with metastatic breast cancer,” he concluded.
Study Details
 Explaining the trial’s rationale, Dr. Mehta noted that the combination of anastrozole (which lowers estrogen levels) and fulvestrant (which downregulates the estrogen receptor) may have additive effects and has been shown to downregulate several resistance proteins in a preclinical model.
Explaining the trial’s rationale, Dr. Mehta noted that the combination of anastrozole (which lowers estrogen levels) and fulvestrant (which downregulates the estrogen receptor) may have additive effects and has been shown to downregulate several resistance proteins in a preclinical model.
The postmenopausal women studied had hormone receptor–positive breast cancer and had not received therapy for metastases. Prior adjuvant tamoxifen was allowed, and prior adjuvant aromatase inhibitor therapy was allowed if completed at least a year earlier.
After stratification by adjuvant tamoxifen receipt, patients were randomly assigned in balanced fashion to treatment with anastrozole with or without fulvestrant. Those in the anastrozole-only arm were strongly encouraged to switch to fulvestrant at progression, and ultimately 41% did.
The patients had a median age of 65 years. Only a minority had received adjuvant tamoxifen (40%), chemotherapy (33%), and aromatase inhibitors (2%).
Trial results showed that patients in the anastrozole/fulvestrant arm had significantly better progression-free survival than their counterparts in the anastrozole arm (15.0 vs 13.5 months; HR = 0.80; P = .007). In subgroup analyses, the difference was significant among those who had not received adjuvant tamoxifen (17.0 vs 12.6 months; HR = 0.74) but not among those who had.
Patients in the anastrozole/fulvestrant arm also had significantly better overall survival (47.7 vs 41.3 months; HR = 0.81; P = .049). This benefit likewise appeared to be restricted to those who had not received adjuvant tamoxifen (47.7 vs 39.7 months; HR = 0.74).
Predictive Factors
Sorting out whether adjuvant tamoxifen is a predictive factor is not straightforward, according to Dr. Mehta. “Prior tamoxifen use is confounded with time between adjuvant diagnosis and metastatic diagnosis,” she explained. “We really need to better understand other possible predictive factors since prior adjuvant tamoxifen could be a false lead from an unplanned analysis.” Benefit was generally similar in subgroups stratified according to a variety of other factors, including age, HER2 positivity, visceral disease, measurable disease, prior chemotherapy, and time since diagnosis.
She added, “If we look at the forest plot, the most benefit was in patients who were diagnosed with breast cancer more than 10 years prior (which included patients who were treated or untreated with tamoxifen). Therefore, the important take-home point is that the trial was powered for all eligible patients, and the progression-free survival and overall survival benefit was significant for all patients in the intent-to-treat analysis who qualified to go on the study.”
“The toxicity of the combination was comparable to single-agent treatment, although grade 5 toxicity was seen only with the combination,” Dr. Mehta reported. Specifically, there were three deaths with the combination, due to pulmonary emboli and cerebrovascular ischemia. Only 1% of patients in the anastrozole group and 3% of patients in the anastrozole/fulvestrant group stopped treatment early because of adverse effects. ■
Disclosure: Drs. Ingle and Pritchard reported no potential conflicts of interest. Dr. Mehta has received research support for a study at UCI by AstraZeneca.
References
1. Mehta RS, Barlow WE, Albain KS, et al: A phase III randomized trial of anastrozole versus anastrozole and fulvestrant as first-line therapy for postmenopausal women with metastatic breast cancer: SWOG S0226. 2011 San Antonio Breast Cancer Symposium. Abstract S1-1. Presented December 7, 2011.
2. Bergh J, Jönsson PE, Lidbrink E, et al: First results from FACT—an open-label randomized phase III study investigating loading dose of fulvestrant combined with anastrozole at first relapse in hormone receptor-positive breast cancer. 2009 San Antonio Breast Cancer Symposium. Abstract 23. Presented December 10, 2009.

