In this installment of The ASCO Post’s Living a Full Life series, guest editor Jame Abraham, MD, FACP, spoke with Derek Raghavan, MD, PhD, FACP, FRACP, FASCO, Founding President of the Levine Cancer Institute. Established in 2011, the Levine Cancer Institute is part of Atrium Health (formerly the Carolinas HealthCare System), a nonprofit health system with more than 500 care locations in North and South Carolina. Dr. Raghavan was recruited to create an innovative model of decentralized cancer care delivery that expands its reach to underserved cancer care populations across the region.
Derek Raghavan, MD, PhD, FACP, FRACP, FASCO

On driving a cab: I drove taxicabs for 3 years during medical school to pay the bills, and in that way I got to meet and chat with a lot of interesting people. That taught me about communicating with various strata in society, which is an important skill in medicine.”
On oncology leadership: “I think you have to understand that as a leader, you have to look after your team and protect them. And it’s good to have a clear mission along with consistency.”
On the future of the field: “We need to be careful not to lose the humanity of oncology when we get consumed with science.”
Dr. Raghavan describes himself as a “diplomatic brat” who was born in Buenos Aires but led a peripatetic life that saw stops in places as far-flung and disparate as Vienna, Austria, Colombo, Sri Lanka, and Karachi, Pakistan. However, his educational journey was largely based in Australia, from grade school on to the University of Sydney, where he attained his Bachelor of Medicine, Bachelor of Surgery (MBBS) degree.
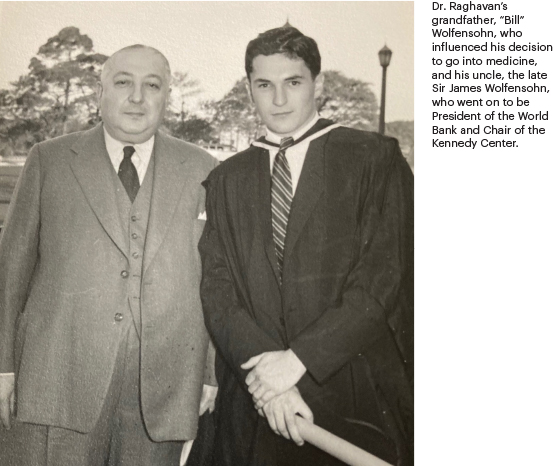
Asked about early influences in his decision to pursue a medical career, Dr. Raghavan replied: “My late grandfather was probably the first person to get me thinking about medicine. He was in Britain and in his first year of medical school when World War I broke out; he volunteered and served in the Middle East, where he saw so much death and destruction that when he returned home, he changed fields—but he always regretted it. So, as a little kid I was told to think about a career in medicine, and that’s pretty much the start of my decision to become a doctor.”
Preferred Internal Medicine Over Surgery
The road to medical school in Australia differs from that in the United States, in that high school students in Australia aspiring to become physicians take entrance exams; if they pass, they go straight to medical school, which is a 5- to 6-year program. As a result, the system produces doctors faster than in the United States. “The first couple of years are of more general stuff—preclinical, lots of science, and you have the option of studying liberal arts and things like that. Then you do a lot of clinical work in the fourth, fifth, and sixth years; you do various clinical rotations,” said Dr. Raghavan.
GUEST EDITOR

Jame Abraham, MD, FACP
The day-to-day routine in the operating theater bored him, as he much preferred the art of clinical problem-solving in internal medicine. For his internal medicine rotation, he got “an absolutely superb mentor,” Dr. John Sands.
“John was a true renaissance man. The Sands family ran the company that makes the Australian version of the board game Monopoly and things like that. They owned a big commercial venture, and John, who was considered the best private practice internist in Sydney at the time, also ran the company in his spare time. But he was an amazing diagnostician, and I thought he trained me very well. I got to work with him as his senior resident for an extended period, and he was a big influencer for me,” noted Dr. Raghavan.
“I’ve always been interested in politics, so I worked in student representation and eventually became President of the Sydney University Medical Society; then I went on to be President of the Residents Club. I’ve also always been an organizer, and the side benefit of that is you could get to know people who not only become friends but also help move your career. And, as an internal medicine resident, I did a lot of moonlighting in the emergency department. So that increased my clinical skills. I also drove taxicabs for 3 years during medical school to pay the bills, and in that way I got to meet and chat with a lot of interesting people. That taught me about communicating with various strata in society, which is an important skill in medicine,” he said.
Other Valued Mentors
During his residency, Dr. Raghavan, who had a fairly strong research background by then, was one of two physicians who were offered a combined fellowship program of immunology and oncology under a new rising star, Australia’s first cancer medicine professor, Dr. Martin Tattersall. “I accepted the fellowship offer, and after completing the first 3-month oncology portion, I decided that’s what I wanted to do with my career. I liked it so much that I called the other fellow and said, ‘Hey, would you like to stay in immunology, and I’ll stay in oncology?’ After I finished my training, at Martin’s suggestion, I went to the Royal Marsden Hospital in Britain, where I saw a huge number of patients. At that time, the British residents were far less experienced in general medicine, so I also taught a training course for residents preparing for their boards,” said Dr. Raghavan.
He continued: “In 1978, I enrolled in a PhD program at the University of London/Institute of Cancer Research, and my thesis was on the functional pathology of germ cell tumors. While in that program, they also allowed me to do some clinical work, and I worked with Dr. Eadie Heyderman, an experimental pathologist, and Dr. A. Munro Neville, Head of the Ludwig Institute for Cancer Research, who became another major influencer in my career.”
Asked about his decision to specialize in genitourinary (GU) oncology, Dr. Raghavan replied: “I worked with Sir Michael Peckham, who was Chairman of the Department of Radiotherapy at the Royal Marsden Hospital, and the late Prof.Tim McElwain, who was Head of Medicine there and a legendary figure at the time in the United Kingdom. They were both international experts in testicular cancer, and they trained me in that field. In fact, I was in one of the first teams to use platinum to treat germ cell tumors. We had thousands of patients with germ cell malignancies at the Marsden, so that kind of pushed me down the pathway of GU oncology.”
While attending a meeting in the south of England, Dr. Raghavan met rising U.S. urologist Dr. Paul Lange, who invited him to work for him at the University of Minnesota, which proved to be another value-added transition in Dr. Raghavan’s career. There he also worked with notables in the field such as Drs. Elwin Fraley and B.J. Kennedy, and shared an office with the late Dr. Nicholas Vogelzang. After a rewarding time in the States, Dr. Raghavan returned to Australia in 1981 and set up the Urological Cancer Research Unit.
“That was kind of a cool experience because, at that time, urologists in Australia were mostly in private practice. So, I set up a research consortium where I had them doing neoadjuvant chemotherapy studies in bladder cancer and new drug investigative studies in prostate cancer, which generated really good data. And our unit become fairly well known because we were able to put patients into studies very readily and participated in a lot of the international studies,” said Dr. Raghavan.
More Career Moves
Seeking more research funding opportunities, Dr. Raghavan was offered a position by Dr. George Bosl, Chief of Medicine at Memorial Sloan Kettering Cancer Center. Although there were many reasons to accept, after experiencing the awful traffic and other quality-of-life problems in New York City, he turned the offer down. However, shortly after, he was recruited to Roswell Park Cancer Institute (RPCI) by oncology luminary Dr. Clara Bloomfield to become Chief of the Division of Solid Tumor Oncology and Investigational Therapeutics. After 6 years at RPCI as Department Chief, another opportunity arose, moving Dr. Raghavan’s blooming career path westward, where he became Chief of Medical Oncology and Associate Director of the Norris Cancer Center at the University of Southern California (USC).
“When I went to USC, I joined SWOG because that was their primary affiliation, and in fact, Dave Crawford was Head of the GU committee and asked me to be his Vice Chair, a role that I held for 10 years. Alexandra Levine was Chief of Hematology; we had adjacent offices and worked very well together. I had a very productive time there,” said Dr. Raghavan.
In 2004, Dr. Raghavan’s oncologic journey took yet another turn in the road, which led to his appointment as Chairman and Director of the Taussig Cancer Center at Cleveland Clinic as well as the M. Frank and Margaret Domiter Rudy Institute (Distinguished) Chair in Translational Cancer Research. Under his leadership, the Institute quickly moved up in the U.S. News & World Report’s national ranking of top cancer hospitals. “While I’m not a big exponent of the criteria used by U.S. News, the ranking really matters. So, we worked very hard as a team and got the ranking from 46 up to number 6 in the country, which was very satisfying for all of us,” said Dr. Raghavan.
During that time, Dr. Raghavan was also responsible for recruiting more than 70 top cancer professionals to the Cleveland Clinic, He was also responsible for major initiatives including early clinical trials in genitourinary cancer, a clinical trial of a circulating tumor cell assay that led to U.S. Food and Drug Administration approval for use as a prognostic tool in prostate cancer, and the establishment of a patient navigation program for underserved Black individuals.
Starting From Scratch
In 2011, Dr. Raghavan became President of Carolinas HealthCare System’s Levine Cancer Institute. “I was assured that they were prepared to put some decent money on the table for program development. When I began my role, there was really nothing much in place other than a very big health-care system with lots of different teams doing bits of oncology—radiation, medical, and so on. During my first meeting with the Chief Executive Officer, I found we were on a different page, as he wanted me to develop a regional cancer center. I told him I wasn’t interested in that as I’d just come from Cleveland Clinic, an internationally known hospital and strong cancer center. So, I sketched out a plan of what I wanted to do, and after reviewing it, they put $500 million on the table for my program development initiative,” he said.
Dr. Raghavan led the development of the Institute’s community-based care efforts to address demographic and geographic disparities in screening and treatment, as well as the acquisition of more first-in-human and phase II clinical trials to advance the study and treatment of cancer. Under his leadership, the Institute launched its first patient navigator academy, which was also one of the first for a health system in the country.
“We’ve run the patient navigator program for 12 years now, and we’ve put a very good proportion of patients on clinical trial. We also published the first Financial Toxicity Tumor Board, and early guidelines for the management of cancer patients during the COVID-19 pandemic. In addition, we had the opportunity to develop the mobile computed tomography scanning unit for lung cancer. I’m presenting our results at the AACR [American Association for Cancer Research] prevention meeting. We’ve done nearly 2,000 scans of heavy smokers who are uninsured, including Black, Native American, Hispanic, and rural poor White individuals. To date, we’ve found 39 lung cancers, two-thirds of which are treatable early-stage disease, which demonstrates the clinical value of mobile scanning,” said Dr. Raghavan.

Balancing Work and Family
Dr. Raghavan noted that his challenging career and his obsessive/compulsive approach to his work have led to certain stresses in his
personal life. “I like married life. I like it so much that I’ve married twice. My first wife, Patricia, is an Australian anesthesiologist. When I was considering a move to Cleveland, we were living in California, and she commented that I worked too many hours. So, when I went on to Cleveland, she didn’t, which was a sad thing. I would never accuse myself of overmuch insight into that sort of thing,” he mused.
“I met my second wife, Judy, in Cleveland after Patricia and I had been divorced for a while. Patricia actually sent me a kindly worded e-mail, noting the things about me that had hurt our marriage, mostly due to my being a workaholic, and she suggested that I share it with Judy, which actually had a beneficial effect on our relationship. So, now I get home on time and I’m a better husband, I’m sure,” said Dr. Raghavan. “I have a wonderful family, three very successful daughters—Nicky, Stephanie, and my stepdaughter, Megan, and beautiful grandchildren. My grandson Finn and I share a birthday, so we have Thomas the Tank Engine and dinosaur parties together.”
How does a super-busy oncology leader decompress? “I always thought when I stepped away from medicine it would be important to have other interests. So, I chaired the Charlotte Symphony Board of Directors for a while, and our Board helped them to become financially secure. And now I’m on the board of the Blumenthal Performing Arts Center in Charlotte, and the World Affairs Council of Charlotte, and a couple of other things. Oh, I also play an atrocious game of golf. So, I keep myself quite busy.”
Words of Advice for Future Leaders
Asked about words of wisdom for future oncology leaders, Dr. Raghavan said: “I think you have to understand that as a leader, you have to look after your team and protect them. And it’s good to have a clear mission along with consistency. I have never liked the idea that many health-care systems have of updating their plan every year or every 2 years. I think you make a really good plan and you stick to it if it’s working, and you tweak it if it isn’t. For example, the plan that I set in Charlotte hasn’t really changed since I arrived because it’s been successful.”
He continued: “I think what matters to me, which is pretty generalizable as a leader, is that you have to be transparent and honest, that my people are loyal, that they know that I’m loyal to them, and that they understand what I’m doing and continue to have that loyalty decades later. I also think you have to set expectations that are reasonable and consistent. And once you set the expectations, then I think you need to hold people accountable. I’m perfectly capable of giving bad news to someone who’s doing bad work. And I think that’s important,” said Dr. Raghavan.
Closing Thoughts
Asked for any final thoughts, Dr. Raghavan responded: “One of the biggest problems that we are dealing with at Atrium Health revolves around our new electronic medical records. We just upgraded, if you can call it that, from a system that wasn’t very doctor friendly to a system that seems less doctor friendly. This whole [electronic medical records] industry is unregulated. They sell these incredibly expensive products, but they don’t have any after-sale service of the type you’d want. And that’s contributing to physician burnout.”
He continued: “So, I’m very worried that the old, most experienced, most faithful, hardworking people are quitting, and they’re being replaced by people with less training and a different work-life balance strategy. And I’m not opposed to the work-life balance strategy; I’m just saying the game is changing, and where that’s going to take us is not clear to me right now. It’s another hurdle, but we’ll manage.”
Dr. Raghavan concluded: “Further, we’ve seen cancer move from empirical wisdom and trying to learn as you go to theoretical considerations that we now can confirm based on our understanding of the genome and its application. We are much more scientific today than we used to be, and that’s paying off. But I also think what we must be careful about is that the fundamentals of good clinical medicine haven’t changed. You have to be an empathetic physician, and you have to really care about your patients. We need to be careful not to lose the humanity of oncology when we get consumed with science. I’m very optimistic about the future, and oncology is a great field.”
Editor’s note: In January 2023, Dr. Raghavan retired from his role as President of Atrium Health Levine Cancer Center, and Dr. Ruben A. Mesa took on the role as President and Executive Director of the Center’s cancer service line. Dr. Raghavan is continuing his clinical work at the W. G. (Bill) Heffner Veterans Affairs Medical Center in Charlotte, where he sees veterans with solid tumors (mostly GU) and trains oncology fellows.
DISCLOSURE: Dr. Raghavan reported no conflicts of interest.

