Despite studies showing the benefits of early palliative care in improving the quality of life of patients with advanced cancer (including reducing symptoms of depression),1 a recent survey of oncologists found there is broad variation in the appropriate utilization of this care.2 Conducted by Cardinal Health Specialty Solutions, the survey polled more than 240 oncologists nationwide—from predominantly (85%) community-based practices—about their perceptions of palliative care and the barriers preventing them from offering timely palliative care services to their patients with metastatic cancer.
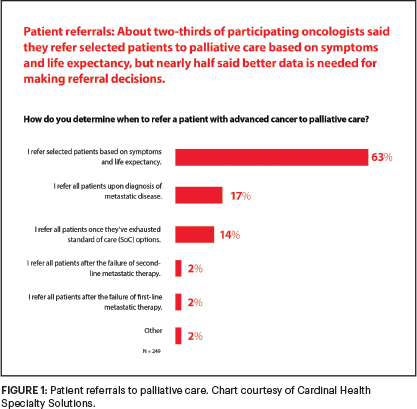
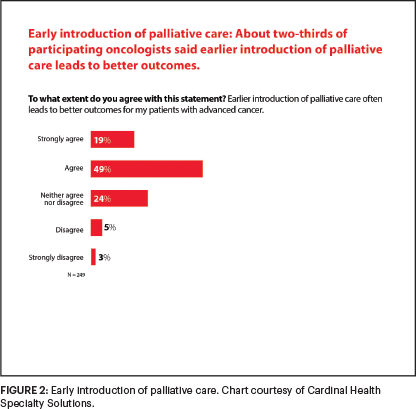
Although ASCO guidelines3 and National Comprehensive Cancer Network (NCCN)4 Clinical Practice Guidelines in Oncology call for palliative care to begin early in the disease course, delivered concurrently with disease-directed, life-prolonging therapies, only 17% of respondents said they refer patients to palliative care at the time of a metastatic cancer diagnosis (Figure 1). And about one in five respondents said they offer palliative care only at the end of life, even though 68% agreed that earlier introduction of this medical care leads to better outcomes (Figure 2).
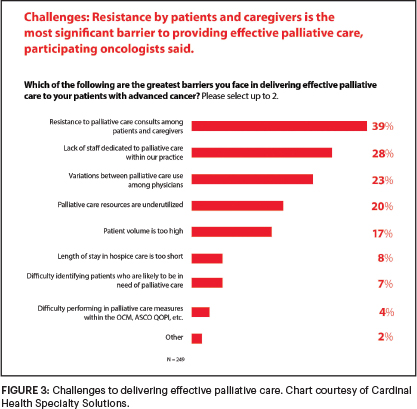
When asked about the greatest barriers to delivering effective palliative care to their patients, 39% cited resistance to palliative care consultations among patients and their caregivers; and 28% said they did not have a dedicated palliative care staff at their practice (Figure 3).
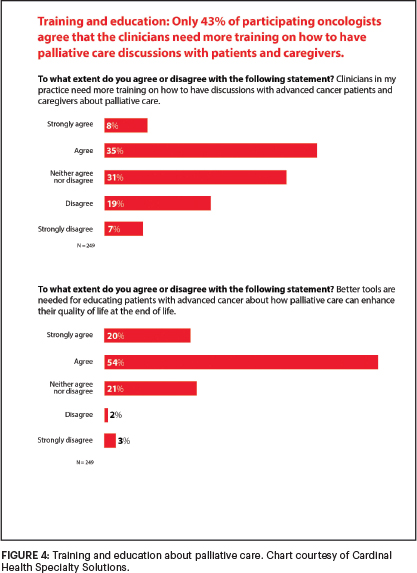
In addition, although only 43% agreed that clinicians need more training on how to have palliative care discussions with their patients with advanced cancer, 74% said that better tools are needed for educating patients about how palliative care can enhance their quality of life at the end of life (Figure 4).
The ASCO Post discussed the findings from the survey with Ajeet Gajra, MD, MBBS, FACP, Vice President and Chief Medical Officer of Cardinal Health Specialty Solutions. He also addressed the implications these results have for patient care.
Overcoming Physician and Patient Resistance to Palliative Care
Why is there such resistance among clinicians, patients, and caregivers to this service? Is there confusion over the definition of palliative care and a conflation with end-of-life hospice care?
These points are valid. I am a medical oncologist trained in palliative care, and although we have come a long way in understanding how and when to provide palliative care and related services, such as hospice care, to patients with cancer, we still need to provide better education to our patients, caregivers, and all oncology clinicians regarding the benefits. My takeaway is that either many community practitioners have not caught up with the palliative care field or the field has not caught up with the needs of these clinicians.

Ajeet Gajra, MD, MBBS, FACP
It is very concerning to me that only 17% of respondents said they refer all patients to palliative care at the time of a diagnosis of metastatic disease. I wish that number were significantly higher.
Our intent with the survey was not to imply that palliative care is the same as hospice care, but I agree that some of the respondents are still equating the two care services. Also, 14% of oncologists said that they refer patients to palliative care only after they have exhausted all standard-of-care options, which is very concerning. Based on the results of our survey, these physicians are waiting until too late in the process for several reasons.
There is still resistance to receiving palliative care among patients and their caregivers, because they think we are giving up on them. Despite appropriate wording and context, I have heard that often from my patients and their family members. We need to do better at getting the message to patients and caregivers that palliative care is not end-of-life care, and it is not hospice care. Also, the results from our survey show that oncologists are not that well informed about the benefits of palliative care in symptom control. Unfortunately, it is leading to significant delays in instituting the care.
What is encouraging about our survey results is that 62% of respondents said they refer patients to in-house palliative care specialists, but that may not mean a physician or an advanced practice provider. It could be a referral to a social worker.
Overcoming the Barriers to Providing Palliative Care
Based on the survey participants’ responses, the barriers to palliative care seem to include a lack of training and staff and a misunderstanding of the term.
I was actually pleased that 43% of oncologists said that more training was needed on how to have palliative care discussions with patients and caregivers. Oncologists, perhaps more than any other medical specialist, are very data driven. And there has been a paradigm shift in the use of palliative care since Dr. Jennifer Temel’s study found that the early introduction of palliative care in patients with advanced lung cancer not only improved their quality of life, but also impacted survival favorably.1 Hopefully, the integration of palliative care early in a diagnosis of metastatic cancer will not only help patients live better, but longer as well.

Clinicians are aware of these benefits but are still not utilizing the service as often as they should. As our survey findings show that oncologists are identifying patients as being resistant to this care. But is it that patients are resistant, or that providers do not know how to broach the subject with their patients? The question is, can we leverage technology to enhance access to and utilization of timely palliative care, especially for practices with limited resources?
Even when both patients and physicians agree to take advantage of palliative care services, there is a lack of access to trained personnel, so all these barriers contribute to suboptimal use of this medical specialty.
Participating in QOPI and OCM Programs to Improve Care
Only 40% of respondents said they participate in -ASCO’s Quality Oncology Practice Initiative (QOPI) program, and just 31% participate in the Oncology Care Model (OCM). And there were mixed opinions about how these programs affected their use of palliative care services (Figure 5). How do you interpret these findings?
Most of our respondents are in community-based practices, and despite these seemingly contradictory findings, there were some positive trends. For example, 60% of those in QOPI programs said the programs resulted in more effective use of palliative care, and 53% said that they led to earlier initiation of the service.
I wish the overall numbers were stronger, but at least it was good to see that the majority of QOPI participants saw the value in using palliative care for their patients. I believe that earlier introduction of palliative care in the course of advanced disease is essential to demonstrate the actual benefit of palliative care. Programs like ASCO’s QOPI and OCM have emphasized earlier integration of palliative care, using it as a quality benchmark.
As intended, these programs not only aim to enhance the overall quality of care delivered but are also meant to be educational. Although the current OCM pilot is ending soon and is expected to be replaced by the next iteration, Oncology Care First, in the near future, QOPI has been a longtime offering. It may be important to demonstrate the “return on investment” to those not engaged in these programs to promote engagement and future participation.
Predicting Patients’ Prognosis
A clear majority of respondents—57%—said oncologists significantly or somewhat overestimate patients’ life spans compared with real-world outcomes. Does that help explain why palliative care is sometimes not offered until the end of a patient’s life?
When a patient’s loved one asks a physician how much time the patient has to live, the physician is usually reluctant to give a number, because the data are not clear on how to accurately determine how long a patient may live. In the real world, patient outcomes are much worse than they are for patients enrolled in clinical trials, because those patients are generally healthier, have fewer comorbidities, and usually live longer.
I think that is a big component of why physicians are hesitant to give patients a prognosis. Also, as physicians, we want our patients to do well and do not want to take away their hope. So, it amounts to talking a fine line between being completely transparent with published survival data for a given malignancy while still offering a hopeful perspective on treatment options and outcomes, and that may well be the art of oncology.
Separating Palliative Care From Hospice Care
What was your greatest takeaway from your findings?
Our results made me realize that although we have made progress in the timely integration of palliative care into standard oncology care, there is still a lot of work to be done on both patient and physician levels to achieve greater use of this specialty care.
Clinicians recognize the benefits of palliation in improving patients’ quality of life and perhaps their longevity. Some are just not able to offer the service because they either do not have the time or staff to provide palliative care medicine to their patients.
GUEST EDITOR

Jamie H. Von Roenn, MD, FASCO
Addressing the evolving needs of cancer survivors at various stages of their illness and care, Palliative Care in Oncology is guest edited by Jamie H. Von Roenn, MD, FASCO. Dr. Von Roenn is ASCO’s Vice President of Education, Science, and Professional Development.
We also have to do a better job of separating palliative care from hospice care, with the emphasis on providing symptom management and supportive care during any stage of disease to improve patients’ quality of life and perhaps survivorship. We have to stop making palliative care synonymous with hospice care. It’s going to take more physician education and training, but we are making progress.
My other takeaway is that more than half of all cancer care in the United States is provided in the community oncology setting.5 These clinicians are busy and are not only engaged in large-volume patient care, but may also be managing the business aspects of their practice. These clinicians may not have the bandwidth to keep up with every quality metric or the newest evidence in palliative care.
Surveys such as ours give a voice to these busy clinicians. But it is critical that their voices and concerns are heard by organizations like ASCO, offering them opportunities for participation and education tailored to their clinical circumstance.
Some examples for better engagement include concise (bite-sized) modules with continuing medical education credit, demonstrating the return on investment if a practice dedicates resources to palliative care. Also, in this new postpandemic world, we have to consider whether there is an opportunity for providing palliative care services using telehealth and leveraging augmented intelligence for the timely identification of patients needing this care and to improving overall palliative care workflow. This may be especially valuable for practices that find access and resources as the major barrier to utilizing palliative care in a timely manner.
DISCLOSURE: Dr. Gajra is Vice President and Chief Medical Officer of Cardinal Health Specialty Solutions, and he owns stock in Cardinal Health.
REFERENCES
1. Temel JS, Greer JA, El-Jawahri A, et al: Effects of early integrated palliative care in patients with lung and GI cancer: A randomized clinical trial. J Clin Oncol 35:834-841, 2017.
2. Cardinal Health: Oncology Insights December 2021: Views From Specialty Physicians Nationwide on Mental Health and Palliative Care Impacts for Patients With Cancer. Available at www.cardinalhealth.com/en/services/specialty-physician-practice/resources/whitepapers-and-downloads/oncology-insights.html. Accessed March 10, 2022.
3. Ferrell BR, Temel JS, Temin S, et al: Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 35:96-112, 2017.
4. Dans M, Kutner JS, Agarwal R, et al: NCCN Guidelines® Insights: Palliative Care, Version 2.2021. JNCCN–Journal of the Comprehensive Clinical Cancer Network. Available at https://jnccn.org/view/journals/jnccn/19/7/article-p780.xml. Accessed March 10, 2022.
5. Community Oncology Alliance: FACT Sheet: What Is Community Oncology? Available at https://communityoncology.org/wp-content/uploads/2017/08/What-is-Comm-Onc.pdf. Accessed March 10, 2022.

