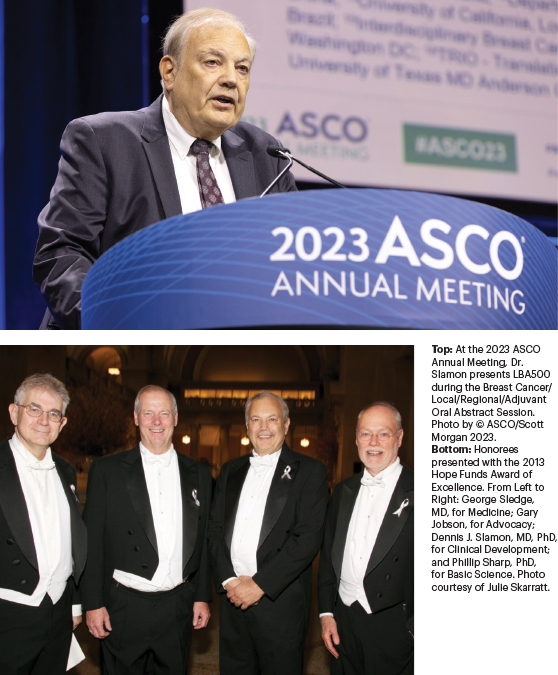
In this installment of The ASCO Post’s Living a Full Life series, guest editor Jame Abraham, MD, FACP, spoke with Dennis J. Slamon, MD, PhD, one of the principals in the discovery and development of trastuzumab—the first monoclonal antibody used against an oncogene that altered our entire approach to cancer therapy. Dr. Slamon serves as Director of Clinical/Translational Research and Director of the Revlon/UCLA Women’s Cancer Research Program at Jonsson Comprehensive Cancer Center.
Dr. Slamon was born and reared in New Castle, a city with a storied past of boom and bust, situated on the banks of the Shenango River in Lawrence County, Pennsylvania.
Dennis J. Slamon, MD, PhD

On the early era of cancer sequencing: “Rather than using cell line models alone, I thought it would be useful to use my clinical training to begin to query and interrogate actual human tumor tissue that was being removed for therapeutic purposes. You could begin to sequence these tumors at the DNA, RNA, and protein levels. Previously, you couldn’t do that with any kind of sophistication.”
On targeting HER2 therapeutically: “When you introduce the HER2 alteration with extra copies to the degree of amplification and get the commensurate overexpression, those cells grew much more rapidly in vitro, were much more tumorigenic in vivo, no longer responded to hormonal manipulation for those that were hormone receptor–positive, and were much more metastatic. That made it a logical target.”
On the importance of good data: “We were told multiple times that ideas we came up with didn’t make sense, and there were preconceived notions that they wouldn’t work, and then there were the data. You have to, at some point, begin to believe the data. We’ve been able to convince other people now that critical analysis of the data, as long as the biology is done really well, can take you in the right direction.”
“When I was growing up, New Castle was a city of about 45,000 people,” he recalled. “But now, it is down to about 25,000, as the steel industry has regressed. My father had worked in the coal mines in West Virginia and Western Pennsylvania and then ended up working in some of the mills in New Castle, and that’s why the family relocated ultimately to New Castle. My mother was a housewife, born and raised in New Castle, Pennsylvania, as well, so they were small-town people.”
A Miner’s Son
Dr. Slamon’s father came to the United States at age 8 from Syria, right before World War I broke out. “My grandfather decided his sons would not fight for the Turkish army, which was allied with the Axis powers at the time [until the collapse of the Ottoman/Turkish Empire in the aftermath of the war, Syria was governed as a group of Ottoman provinces], so he immigrated,” he related. “They didn’t speak English, weren’t educated, and were not literate even in their native language. The only work they could get was in the mines. They realized it was a land of opportunity, and that’s what drove them to immigrate.”
“I saw how hard my dad and his brothers worked,” Dr. Slamon continued. “They were all involved in the coal mines and then ultimately in the steel and paper mills. They worked very hard to support the family, big believers in the American dream, and provided for their family and their children, making sure they were educated and always supported to pursue whatever excited them.”
As for Dr. Slamon’s mother, she was a first-generation immigrant. Her parents were also from Syria, but she was born in this country. “It was that immigrant mentality of doing things in a new country, where opportunity abounded, that drove them to say this is the right place to have a family and then to engender that work ethic in their kids to go forward. It was a positive influence,” he shared.

Early Influences and Education
Asked about any early influences on his decision to pursue a career in medicine, Dr. Slamon responded: “There were two people. The family pediatrician was someone who had a big influence on how I looked at doctors. His name was Abraham Newmark, and he was a really great guy. He was an old-time pediatric practitioner who made house calls and practiced medicine the old way. And it made a real impression on me, my parents, and my siblings. It seemed like a very exciting and interesting profession to be able to come in and help people when they were ill. The second person was a student biology teacher in high school, who actually did more than just read from the textbook; he got most of the class, and certainly me, excited about biology.”
After graduating from high school, Dr. Slamon attended Washington and Jefferson College, a liberal arts college in a small community in the Western Pennsylvania Rust Belt called Washington. “After getting my bachelor’s degree in biology, I wanted to pursue joint degrees and was fortunate enough to be accepted into a graduate and a medical program at the University of Chicago. I started there in 1975. I finished my graduate work; did my MD and my PhD as part of that program; and then stayed on there for internship, residency, and chief residency. All told, I spent 10 years in Chicago at the University of Chicago. I was actually the first person in my family to go to college,” he said.

Road to Oncology
According to Dr. Slamon, his intense interest in biology was the driver in his early path toward a career in oncology. “I had a passionate interest in medicine and the biology of diseases,” he shared. “What I was able to see when I was training in medical school is the biology of cancer was one of the most interesting and exciting things I was exposed to, and it was in the very early period of medical oncology. Combination chemotherapy was just coming into its own in terms of treatments for some of the cancers after Vince DeVita’s work on combination chemotherapy for Hodgkin lymphoma. As you know, the next 40 years were dominated by various things that did that, but at about the same time in the early 1980s, it became known there might be these things known as oncogenes carried by acutely transforming retroviruses, and their oncogenic potential was profound.”
Dr. Slamon continued: “Sequencing wasn’t widespread at the time, and the first viral sequences didn’t come out until around that time; no one knew why these agents were so oncogenic, until finally it was identified they were carrying genetic information that was very progrowth stimulatory. And, ultimately, the observations made by a couple of investigators (including Mike Bishop and Harold Varmus) that the sequences these viruses were carrying were actually sequences stolen from normal mammalian cells, avian cells for those that infected avian species. And those sequences were sequences that were contained in all these normal tissues because they were important in regulating growth. However, these acutely transformed retroviruses, given the fact that they were retroviruses and their lifecycle took them through the DNA, would occasionally pirate or steal these sequences that were growth regulatory. And when they were under the control of the viral promoters not expressed in their normal context, you’ve got these cancers that these experimental viruses could cause—more oncogenic than radiation, more oncogenic than any kind of chemical carcinogens we knew about at the time. It was pretty impressive, and that whole era is when the field of oncogenes and gene sequences and alterations in genes began to be known as an incredible etiologic factor in oncology. It’s all second nature to everybody today, but back then, it was pretty exciting and new.”
GUEST EDITOR

Jame Abraham, MD, FACP
HER2: A New Way to See Breast Cancer
When the discussion turned to a deeper dive into his oncology path, eventually leading to his groundbreaking work in HER2, Dr. Slamon continued: “I decided to do a fellowship training at UCLA. It was a hematology-oncology combined fellowship, which I liked. There was experience in solid oncology, as well as hematologic lymph disease and bone marrow transplantation. I had a job offer to come back to Chicago when I was finished with fellowship training. And at that time, I had every intention of doing that because I really enjoyed my time at the University of Chicago. But after I finished my clinical part of my fellowship training, the lab part came up next; then I got back into the lab and learned that, during all my training, the molecular era had been born in terms of cloning techniques and sequencing. And in doing that, I learned about these genes, oncogenes, and became very excited about them and started to interrogate them in human tumors. So, rather than using cell line models alone, I thought it would be useful to use my clinical training to begin to query and interrogate actual human tumor tissue that was being removed for therapeutic purposes. Now, you could begin to sequence these tumors at the DNA, RNA, and protein levels. Previously, you couldn’t do that with any kind of sophistication. It was really the early era of sequencing.”
Dr. Slamon continued: “The first paper where I really did some of this work was a study of the expression of oncogenes, about 11 of them, in various human tumor tissues, and I started to develop banks of human tumor tissues. In 1984, I published my first paper in Science about expression in tumor tissue and differential expression in tumor vs normal adjacent tissue. That was exciting to me at the time. I ended up identifying that HER2 alteration in the lab by interrogating a cohort of breast cancer specimens removed surgically for therapeutic purposes and looking at the DNA.”
Although Dr. Slamon admits it was using a very primitive technology by today’s standards, it was technology that would allow the interrogation of DNA. “I found that about 20%, 25% of these breast cancer specimens had amplification of a region of chromosome 17 in the long arm,” he explained. “And, in that region, the HER2 gene was present.”
Next, Dr. Slamon collaborated with Gary Clark, who was part of the McGuire Group at San Antonio. “I got a bunch of tissues that had long-term follow-up; when these tumors were amplified, they tracked with very aggressive clinical behavior with shorter disease-free and overall survival. That’s what took me off on the whole field of HER2 and breast cancer. It was really a fishing expedition looking at different cancers and different oncogenes that led me to that observation.”
Big Leap Forward
Although the story of the development of trastuzumab reads like a medical tour de force, Dr. Slamon credits old-fashioned science problem-solving. “We’ve been given a lot of credit for some really unique thinking, but it wasn’t so unique; it was really pretty logical. We saw the correlation with outcome, and this alteration was prognostic. It was even as prognostic and independent of other things we traditionally used, such as size and grade and number of nodes, but here was this molecular alteration that could tell us the very same information. This is way before Oncotype and MammaPrint, or any of those technologies, were around. It was just looking at a single gene, and we saw this correlation that led to the logical question: Is this simply a marker of aggressive tumors and tracks with them, or is it tracking with an aggressive phenotype because it plays some role in causing that phenotype? And that’s where the training I had in Chicago came into play because my PhD work was in cell biology,” he commented.
“So, it was back to the lab to take cells,” Dr. Slamon continued, “human breast cancer cells, that did not have the alteration, introduce the alteration at the same level that you see in clinical material, and ask, would the cell behavior change? We found that when you introduce the HER2 alteration with extra copies to the degree of amplification and get the commensurate overexpression, those cells grew much more rapidly in vitro, they were much more tumorigenic in vivo, they no longer responded to hormonal manipulation for those that were hormone receptor–positive, and they were much more metastatic. This indicated that it was tracking with a bad outcome because it was playing some role in causing it. That made it a logical target, and that’s what led to thinking about how to go after it therapeutically.”
Finding a Partner in Industry
Drug development is a highly collaborative enterprise, and Dr. Slamon found a key collaborator at Genentech. “At the time, our lab was not doing any of our own generation of antibodies. This was the early days of monoclonal antibodies, not the earliest days, but still pretty early. But there were companies very good at it, so we started to collaborate with them,” he explained.
When they found the HER2 alteration, an initial collaboration started with Axel Ullrich, who had cloned the gene and was at Genentech, according to Dr. Slamon. “The sequence probes I got were from Axel. He gave me six different probes he had recently been involved in cloning that included HER2. And he had called that HER2 because it looked like HER1, or the EGF receptor. Using low stringency hybridization in a placental library, he pulled out a sibling, something that looked very close to the EGF receptor but was unique, and that was HER2,” he explained.
Dr. Slamon continued: “No one knew anything about this biology at the time. But one of the things you do when you identify a new gene, you express it, make the protein, and make antibodies against the protein so you can study it. Brian Finley at Genentech was working with Axel and had done that. So, I asked him for some of those antibodies, and we put them into our in vitro studies for those engineered cells we had made HER2-positive, as well as natural cells that were HER2-positive; and we found, sure enough, it would suppress their growth.”
According to Dr. Slamon, they moved from the in vitro studies to in vivo studies and saw that as well. “This is how everything got started to think about antibodies,” he explained. “We worked with Amgen, who also had antibodies against this protein. When they identified new genes or saw new genes in the literature, they would make antibodies, too, to begin to study the protein to understand its biology. So, we got some of their antibodies. We got some from a third company called Berlex Laboratories. Then we tried to generate some of our own, but again, we weren’t as sophisticated as our industry colleagues.”
Dr. Slamon continued: “Then we found that several antibodies from different sources could inhibit the growth, but it was really a small core of people at Genentech who became interested in pursuing this further, because there was bias against antibodies, as you may remember. It took a lot of convincing and a lot of data coming from the preclinical lab, both from us and from small groups at Genentech involved with us, that finally talked the company into producing a humanized version of the antibody to test in the clinic. So, it was this collaboration that led us to little clinical trials that we were fortunate enough to be able to execute the initial phase I study, the first patients treated, the phase II and phase III studies, and the initial study that got the drug approved.”
Their findings led to the first clinical trials of trastuzumab at UCLA in 1992 and 1993. These early trials were followed by additional trials and finally U.S. Food and Drug Administration approval in 1998.
Intersection of Industry and Academia
When Dr. Abraham asked about the intersection of industry and academic medicine in the drug development process, Dr. Slamon responded: “For a long time, industry had its own big science groups that were doing their own internal research, and they still do. But now, more than ever, they are looking at academic labs, small labs for ideas and findings and data they could then bring into their companies to go further. Academic and industry collaborations are very important, very useful, and continue to be something people should explore in the future.”
Dr. Slamon noted that one true key is to have really good data and follow them. “We were told multiple times that ideas we came up with didn’t make sense, and there were preconceived notions that they wouldn’t work, and then there were the data. And you just look at the data, and they keep showing the same thing. You have to, at some point, begin to believe the data, as opposed to your preconceived notions, and I think that is what has carried us a long way. It’s not that we haven’t had wrong ideas—we’ve had plenty—but then the data tell us which direction to go in. And we’ve been able to convince other people now that critical analysis of the data, as long as the biology is done really well, can take you in the right direction,” he said.
Decompression Time
How does a super-busy oncology researcher wind down from the rigors of his career? “I really enjoy fishing and doing things outdoors, especially in the mountains in terms of backcountry exploration. I have two grown children and grandchildren, so they are a really exciting part of life that I find every bit as rewarding as parenting. I’ve had a wonderful life and have been blessed, for sure. I’ve had great colleagues, great friendships outside of medicine, and a family who’s been very supportive of my academic pursuits.”
Words of Advice
Asked to share a word or two of advice for young doctors thinking about pursuing a career in oncology, Dr. Slamon said: “Obviously, I’m biased, but I think oncology is the most exciting field in medicine, combining cutting-edge science, research, and intimate patient care. Cancer has taught us so much and led the way in molecular medicine and molecular therapeutics in ways that surprised everyone. It went from a field where we were pretty primitive in our approaches to treating a disease to being relatively sophisticated. There’s still a lot more to do, and with the technology we have available to us today, it’s an exciting time for young people to become involved in cancer and oncology. I know ASCO plays a big role in trying to excite and engage young investigators, and that’s a very positive thing to do. I encourage people to jump in, get involved, and enjoy the ride.”
DISCLOSURE: Dr. Slamon has served in a leadership role for 1200 Pharma, BioMarin Pharmaceutical, and Torl Biotherapeutics; has stock and other ownership interests in Amgen, BioMarin Pharmaceutical, Merck Sharp & Dohme, Pfizer, Seagen, and Vertex; has received honoraria from Novartis; has served as a consultant or advisor to Eli Lilly, Novartis, Pfizer, and Seagen; has received research funding from Novartis and Pfizer; and has received reimbursement for travel, accommodations, and expenses from BioMarin Pharmaceutical, Novartis, and Pfizer.

