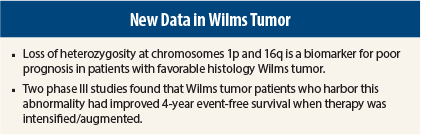
Data from two phase III studies led by the Children’s Oncology Group show that augmenting or intensifying therapy for children with high-risk Wilms tumor improved relapse-free survival. These children are deemed to be at high risk due to a specific chromosomal abnormality that confers worse prognosis: loss of heterozygosity for chromosomes 1p and 16q.
“Intensification of therapy upfront is not advisable for all patients with Wilms tumor. We have identified a biomarker for high-risk patients at diagnosis [loss of heterozygosity for chromosomes 1p and 16q], and in these patients, intensification of therapy improves outcomes,” said lead author David B. Dix, MD, of British Columbia Children’s Hospital in Vancouver, Canada, at a press briefing held in advance of the ASCO Annual Meeting, where the new data was presented.1 “We are encouraged that augmentation of therapy can overcome a known adverse biomarker.”
Wilms tumor is a rare form of kidney cancer that typically occurs in children under the age of 5 years. About 500 new cases are diagnosed each year in North America. Children with favorable-histology Wilms tumor account for about 75% of childhood kidney cancers, and only about 5% of these patients harbor loss of heterozygosity for 1p and 16q.
Study Details
The AREN0532 and AREN0533 trials enrolled 1,134 patients, 35 with favorable-histology stage I/II Wilms tumor and loss of heterozygosity for 1p and 16q and 52 who had stage III/IV favorable-histology stage I/II Wilms tumor and loss of heterozygosity for 1p and 16q.
These two groups of patients were treated differently according to stage. The augmented regimens were as follows: Stage I/II patients received vincristine, dactinomycin, and doxorubicin (Regimen DD4A), while stage III/IV patients received those three drugs alternating with four cycles of cyclophosphamide/etoposide and radiotherapy (Regimen M).
Previous studies showed that stage I/II patients with loss of heterozygosity treated with standard therapy (vincristine/dactinomycin) had a 4-year event-free survival rate of 74.9%, and stage IIII/IV patients with loss of heterozygosity treated with standard therapy (those two drugs plus doxorubicin and radiotherapy) had a 4-year event-free survival rate of 65.9%.
Median follow-up was 3.6 years. By augmenting the regimens and targeting them to patients with high-risk Wilms tumor (favorable histology but loss of heterozygosity for 1p and 16q), 4-year event-free survival was boosted from 74.9% to 83.9% in stage I/II patients and from 65.9% to 91.5% in stage III/IV patients.
“These studies suggest that augmentation of therapy markedly improves outcomes for patients with advanced disease and this abnormality. Due to smaller numbers in the study sample, the benefit [of augmentation therapy] is less clear for those with lower-stage disease but suggests improved outcome,” he commented.
Adverse Events
The treatment was well tolerated overall, and toxicities were manageable, Dr. Dix said. In earlier-stage patients, augmented therapy did not lead to a significant increase in adverse events over the short term. In later-stage patients, myelosuppression was the most common severe adverse event associated with the augmented regimen, reported in 60% of patients.
Regimen M used to treat later-stage patients is associated with a risk of reduced fertility, but according to the authors, this regimen spares some patients from having to undergo intensive relapse therapy. The authors recommend that oncologists have a clear discussion outlining risks and benefits of augmented therapy for higher-risk patients with loss of
heterozygosity.
Testing for loss of heterozygosity (for 1p and 16q) is considered the standard of care and is performed at the Children’s Oncology Group Biopathology Center and several other centers, Dr. Dix said.
Poor-Prognosis Patients
Commenting on these findings, ASCO President-Elect Julie M. Vose, MD, said, “It’s very encouraging that we’re making progress even for kids with a rare, high-risk form of this disease. The ability to easily identify a small subset of patients with a poorer prognosis means these children can receive treatment that’s right for them, while decreasing side effects for lower-risk patients. And that means a better shot at surviving their cancer.”
She added, “It would not be possible to do this study without federally funded research. The goal of this study is to use genetic testing to escalate therapy in high-risk patients and de-escalate it in low-risk patients.” ■
Disclosure: The National Institutes of Health funded this study. For full disclosures of the study authors, visit meetinglibrary.asco.org.
Reference
1. Dix DB, Fernandez CV, Chi Y-Y, et al: Augmentation of therapy for favorable histology Wilms tumor combined with loss of heterozygosity of chromosomes 1p and 16q: A report from the Children’s Oncology Group studies AREN0532 and AREN0533. 2015 ASCO Annual Meeting. Abstract 10009. Presented June 1, 2015.