The ASCO Post’s Integrative Oncology series is intended to facilitate the availability of evidence-based information on integrative and complementary therapies sometimes used by patients with cancer. In this installment, Jun J. Mao, MD, MSCE, Guest Editor of the Integrative Oncology series, and Yen Nien (Jason) Hou, PharmD, DiplOM, LAc, focus on a novel herbal oncology program, which may help to serve as a prototype for other cancer care providers as well as inform future research to expand the evidence base around the safe and effective use of herbal supplements to improve patient outcomes.

Jun J. Mao, MD, MSCE

Yen Nien (Jason) Hou, PharmD, DiplOM, LAc
Overview
Use of herbs and supplements continues to be prevalent among patients with cancer. Nearly 60% self-medicate with herbal supplements for symptom control and for enhancing quality of life.1-3 However, very few patients disclose herbal use to their health-care providers, and unsupervised use may lead to undesirable effects and herb-drug interactions. This is especially concerning in patients receiving active treatment. Documented herb-drug interactions include those with chemotherapy agents,4 anticoagulant/antiplatelet drugs,5 immunosuppressive agents,6 and hormonal therapies,7 rendering some medications less effective and amplifying the effects of others. Many health-care providers are also ill-equipped to have useful discussions around herbal use due to lack of knowledge or training.8
Overview of the Herbal Oncology Program
To address the two vital gaps—unmet patient needs for symptom control and inadequate patient-provider communication about herbal use—the Integrative Medicine Service (IMS) at Memorial Sloan Kettering Cancer Center (MSK) initiated an herbal oncology program in 2019. This program involved establishing an herbal formulary and dispensary to offer patients quality-controlled traditional Chinese medicine (TCM) formulas with evidence of safety and preliminary efficacy for common cancer symptoms, such as constipation or diarrhea,9,10 insomnia,11 and mood disorders.12
The formulary was set up after thorough discussions among integrative medicine practitioners, TCM oncologists in China (where TCM herbs and formulas are often used to manage cancer-related symptoms), review of classic herbal medicine textbooks, and by conducting systematic reviews of the available literature.9,10,13 Herbal products were procured following a rigorous quality assurance process by an IMS pharmacist trained in conventional pharmacy and TCM herbology. The procedures followed for stocking, prescribing, and dispensing herbal products were identical to those for prescription drugs.
Another vital component of the herbal oncology program was discussing herbal medicine at all integrative oncology consultations to facilitate shared decision-making around herbal use. When an IMS physician determined that herbal medicines may benefit a patient, the potential benefits outweigh the potential risks, and better alternatives are lacking, he or she would recommend herbal prescription after discussing the rationale with the patient, looping in the oncology team as needed.
The prescriptions were dispensed through MSK’s outpatient pharmacy. Patients also had the option of receiving their prescriptions by mail. In addition, the IMS pharmacist was available to counsel patients with any additional questions about the prescriptions. Although herbal medicines are presently not covered by insurance, in many cases, patients used a pretax health savings account or a flexible spending account to pay for the prescriptions.
Implementation and Evaluation
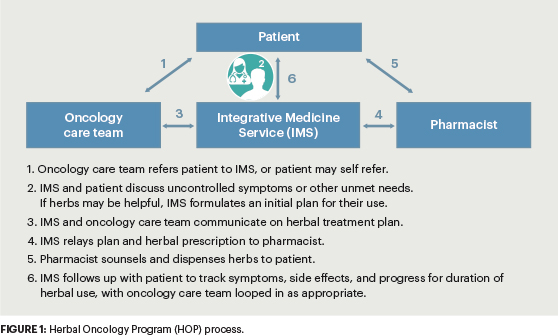
The workflow and process were tested over the course of a year before the herbal oncology program was implemented (Figure 1). A data tracking system was developed to record detailed prescription patterns, fill patterns, and address potential adverse events.
Following receipt of institutional review board approval, a retrospective chart review of all patients who participated in the program from February 1, 2019, to January 31, 2022, was conducted. The review included symptoms and other concerns that motivated patients to seek herbal products, types, and numbers of dispensed TCM herbal prescriptions, and demographics. A brief 10-question survey was sent to the participants who received an herbal prescription between May 1 and August 31, 2021, to assess their experiences with the herbal oncology program.
Key Findings
A total of 1,266 herbal prescriptions were dispensed to 851 patients being treated for a wide range of cancers; 712 (84%) were undergoing active treatment. The majority were female (606, 71%), White (594, 70%), and publicly insured (498, 59%), and the median age was 61 (18–98 years). Common symptoms addressed with the herbal medicines were gastrointestinal (467, 37%); pain (353, 28%); and treatment-related fatigue, sleep, and mood disorders (346, 27%).
Among the 269 patients invited to participate in the survey, 107 (40%) provided specific feedback, as detailed here:
- Many patients (70.9%) reported being satisfied with the effectiveness of herbal prescriptions in controlling their symptoms.
- Few patients (6.7%) experienced mild adverse effects, which included constipation, bloating, heartburn, acid reflux, and skin discoloration and peeling. All adverse effects resolved after herbal use was stopped.
- Most patients (86.5%) found obtaining herbal medicines through the dispensary “somewhat to extremely easy.”
- Nearly all participants (80.4%) rated the ability to discuss herbal medicines with an integrative medicine provider as “very to extremely important.”14
Concluding Thoughts
Patients with cancer increasingly resort to herbal supplements for relief from challenging symptoms. The findings of this study support the feasibility of incorporating herbal medicines into an academic oncology setting. Patient satisfaction with the herbal oncology program was high, with few adverse effects. Of note, the open communication and shared decision-making facilitated by the herbal oncology program—highly valued by most patients—helped avert the detrimental effects from unsupervised herbal use.
Our herbal oncology program may help to serve as a prototype for other cancer care providers in the United States and elsewhere. Further, the patterns of herbal prescriptions may inform future research to bolster the evidence base around the safe and effective use of herbal supplements for improving patient outcomes.
DISCLOSURE: Dr. Mao has received institutional research funding from Tibet Cheezheng Tibetan Medicine Co Ltd. Dr. Hou reported no conflicts of interest.
REFERENCES
1. Correa-Velez I, Clavarino A, Eastwood H: Surviving, relieving, repairing, and boosting up: Reasons for using complementary/alternative medicine among patients with advanced cancer: A thematic analysis. J Palliat Med 8:953-961, 2005.
2. Gupta D, Lis CG, Birdsall TC, et al: The use of dietary supplements in a community hospital comprehensive cancer center: Implications for conventional cancer care. Support Care Cancer 13:912-919, 2005.
3. Evans M, Shaw A, Thompson EA, et al: Decisions to use complementary and alternative medicine (CAM) by male cancer patients: Information-seeking roles and types of evidence used. BMC Complement Altern Med 7:25, 2007.
4. Ambrosone CB, Zirpoli GR, Hutson AD, et al: Dietary supplement use during chemotherapy and survival outcomes of patients with breast cancer enrolled in a Cooperative Group Clinical Trial (SWOG S0221). J Clin Oncol 38:804-814, 2020.
5. Ulbricht C, Chao W, Costa D, et al: Clinical evidence of herb-drug interactions: A systematic review by the natural standard research collaboration. Curr Drug Metab 9:1063-1120, 2008.
6. Deng G, Lin H, Seidman A, et al: A phase I/II trial of a polysaccharide extract from Grifola frondosa (Maitake mushroom) in breast cancer patients: Immunological effects. J Cancer Res Clin Oncol 135:1215-1221, 2009.
7. Liu B, Edgerton S, Yang X, et al: Low-dose dietary phytoestrogen abrogates tamoxifen-associated mammary tumor prevention. Cancer Res 65:879-886, 2005.
8. Lee RT, Barbo A, Lopez G, et al: National survey of US oncologists’ knowledge, attitudes, and practice patterns regarding herb and supplement use by patients with cancer. J Clin Oncol 32:4095-4101, 2014.
9. Yang M, Feng Y, Zhang YL, et al: Herbal formula MaZiRenWan (Hemp Seed Pill) for constipation: A systematic review with meta-analysis. Phytomedicine 82:153459, 2021.
10. Wang H, Hou YN, Yang M, et al: Herbal formula Shenling Baizhu San for chronic diarrhea in adults: A systematic review and meta-analysis. Integr Cancer Ther 21:15347354221081214, 2022.
11. Song MF, Chen LQ, Shao QY, et al: Efficacy and safety of Jiawei Suanzaoren Decoction combined with lorazepam for chronic insomnia: A parallel-group randomized controlled trial. Evid Based Complement Alternat Med 2020:3450989, 2020.
12. Wang Y, Shi YH, Xu Z, et al: Efficacy and safety of Chinese herbal medicine for depression: A systematic review and meta-analysis of randomized controlled trials. J Psychiatr Res 117:74-91, 2019.
13. Yang M, Li SQ, Smith CM, et al: Tibetan herbal pain-relieving plaster for low back pain: A systematic review and meta-analysis. Biomed Pharmacother 140:111727, 2021.
14. Hou YN, Chimonas S, Gubili J, et al: Integrating herbal medicine into oncology care delivery: Development, implementation, and evaluation of a novel program. Support Care Cancer 31(2):128, 2023.

