The Centers for Medicare and Medicaid Services projects that U.S. health-care spending will reach $4.3 trillion and account for 19.3% of the nation’s gross domestic product by 2019.1 Although cancer care represents a small fraction of overall health-care costs, the cost of cancer care is rapidly increasing, now estimated to reach $158 billion in 2020—an increase of 26% over just a decade.2
These expenditures are driven by the increasing prevalence of cancer due to the overall aging of the population and the introduction of costly, but hopefully more effective, new drugs as well as improved techniques in radiation therapy and surgery, resulting in more patients continuing on treatment for longer periods of time. Also contributing to rising costs are physician reimbursement models that reward the quantity rather than the quality of care delivered, the often inappropriate use of tumor-directed therapy near the end of life, and the sometimes desperate hopes and unrealistic expectations of patients and family members that lead clinicians to offer certain options despite lack of clear evidence of clinical benefit.
Cost vs Value
Rising health-care costs are distributed throughout the broader economy by causing higher insurance premiums, increased cost shifting to patients in the form of higher deductibles and copayments, higher taxpayer burden, and stagnant wages. A resulting concern is that health care will become less and less affordable for Americans unless steps are taken to curb current trends.
Indeed, health-care expenditures are now cited as a major cause of personal bankruptcy, and the term “financial toxicity” has been introduced to describe the financial distress that now often accompanies cancer treatment. Patients experiencing high out-of-pocket costs have reported reducing their spending on food and clothing, reducing the frequency with which they take prescribed medications, avoiding recommended procedures, skipping physician appointments, and having poor quality of life. But cost is only one component of a complex calculus that must weigh health outcomes against dollars spent to assess the true value of health care.
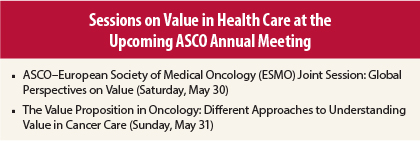
Value must be considered from the varying perspectives of consumers of health care, providers of health care, payers for health care, purchasers of health care, and innovators of health-care products. Many of these perspectives will be examined in two sessions at the upcoming 2015 ASCO Annual Meeting (see figure in sidebar).
Consumer’s View
In the United States, consumers with insurance have typically been shielded from the full costs of their health care, as direct out-of-pocket costs are only a fraction of the total cost of their care. But as costs continue to rise, even insured patients are beginning to struggle with monthly out-of-pocket expenditures of thousands of dollars.
For consumers, value is defined primarily by health outcomes, eg, cure of disease, longevity, relief of symptoms, resumption of usual daily activities, improvement in quality of life, and achievement of personal goals. Value is often defined in very personal ways, depending on individual preferences, work requirements, comorbidities, family circumstances, and financial realities.
Provider’s View
Oncologists and other members of the cancer care team have a primary responsibility to deliver high-quality, evidence-based, efficient care to their patients. For providers, value can be created through a shared decision-making process that lays out prognosis, goals of treatment, treatment options, and expected benefits and risks in the context of the patient’s preferences, values, and personal goals.
To make informed choices, patients also need information about the costs of their medical care and the relationship between the costs they will incur and the benefits they will receive for different treatment options. ASCO’s value framework, soon to be released for public comment, will provide the foundation for a tool that will help doctors and patients assess the relative value of cancer therapies based on efficacy, side effects, and cost.
Payer’s View
Payers focus largely on the distribution of illness and wellness in the covered population, reduction in use of expensive treatments and procedures not supported by medical evidence, elimination of inefficiencies in health-care delivery systems that lead to duplication of services, and enhanced communication among providers and between providers and patients to reduce unecessary emergency room visits or hospitalizations. For payers, achieving high value care depends not only on improving health outcomes but also on reducing waste, improving efficiency, and increasing access to the primary health-care team, all of which tend to drive down costs.
Purchaser’s View
Purchasers of health care, whether governments or private companies, often consider multiple factors when deciding whether or not to introduce a new product or service as an option for their population. Purchasers typically have a fixed and limited budget, and considerations often include the competing health-care needs of the population, the extent of unmet medical need for a condition, available alternatives, and overall affordability of a new treatment as well as its incremental benefit and toxicity. Indeed, most developed countries other than the United States employ health technology assessments provided by a government-sanctioned entity to determine the value of a new therapeutic option and use this assessment to engage in price negotiations with the product manufacturer to obtain the lowest cost and best value.
Innovator’s View
For product innovators, value is determined in the context of research and development investment and shareholder expectations. From the innovator’s perspective, value is often assessed over the life cycle of the product, as product performance varies across patient populations, by line of therapy, and based on whether a biomarker selection strategy is employed.
Pricing and reimbursement typically depend on marketplace competition, region of the world, and duration of patent exclusivity and less so on treatment indication and magnitude of incremental benefit achieved. To be sure, cancer drugs take years to develop and billions of dollars in research investment, and for every success, there are dozens of failures. Yet even drugs that successfully reach the market sometimes produce only modest incremental improvements in clinically important endpoints—nevertheless, they still enter the market with extraordinarily high prices.
Optimizing Value
For all stakeholders, the definition of value ultimately comes down to the price that must be paid to achieve meaningfully improved health outcomes at the level of individual patients or for the broader population of affected individuals. Optimizing the value of a new product begins with innovation to address an unmet medical need followed by defining and achieving clinically meaningful improvements in health outcomes through well-designed and efficiently conducted clinical trials. Effectiveness research is essential to determine how well the new product performs compared to available alternatives and in more diverse populations than those typically included in the clinical trials used to establish efficacy.
Patient goals, preferences, and choices shape the real-world experience with a new product, and the direct and indirect costs of treatment to patients and their families impact its widespread adoption. Until their value is clearly established, new and costly products should be deployed judiciously by the medical community after careful consideration of the goals of treatment; available options; and the unique needs, preferences, and goals of individual patients.
Research in many domains is necessary to improve the assessment of the value of new cancer treatments. New clinical efficacy endpoints—both provider- and patient-reported—that accurately describe how a patient feels and functions must be developed and should reflect outcomes of value to patients other than survival, particularly in noncurative settings. Better predictive biomarkers can transform a drug of modest efficacy in an unselected population to one of high efficacy in a biomarker-defined subgroup and thereby contribute to improving the value of a treatment.
Regulatory and policy initiatives (such as adaptive licensing, value-based insurance, and indication-specific pricing, which impact marketing approval, reimbursement, and price, respectively) based on treatment effectiveness all deserve careful consideration. Further research must also be conducted to determine the impact of these initiatives on aligning cost with benefit while insuring patient access to life-prolonging therapies and continuing innovation in product development.
All Stakeholders Accountable
All stakeholders need to accept accountability for improving the value of cancer treatment. Providers need to practice evidence-based medicine focused on quality rather than quantity of care and engage in shared decision-making with their patients. Patients need a better understanding of treatment options, potential outcomes, and costs to help establish realistic goals.
Industry needs to responsibly price products to support true innovation but ensure access. Payers need to make well-informed, fair, and transparent coverage decisions. Purchasers of health care need to demand that the cost of a given intervention bears a relationship to the beneficial impact it has on the patients who receive it.
Together, we can and we must ensure that all patients have the opportunity to achieve optimal outcomes at affordable costs—ie, that patients receive high-value, not just high-cost, cancer care. ■
Disclosure: Dr. Schilsky reported no potential conflicts of interest.
References
1. Centers for Medicare and Medicaid Services: National Health Expenditure Projections 2010-2020. Available at www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/proj2010.pdf. Accessed April 15, 2015.
2. Mariotto AB, Yabroff KR, Shao Y, et al: Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst 103:117-128, 2011.
Dr. Schilsky is Chief Medical Officer of the American Society of Clinical Oncology.