With a population under half a million people, Brunei Darussalam is a small equatorial nation in Southeast Asia. Bordered by the South China Sea on the north, Brunei Darussalam is surrounded on all other sides by Malaysia, which separates the nation into two noncontiguous parts.
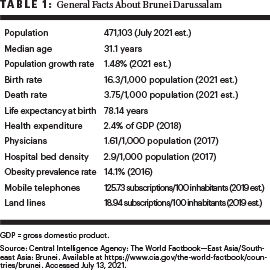
Nearly two-thirds of the population of Brunei Darussalam are Malay, including ethnic Malays as well as indigenous groups; the remainder of the population is Chinese, non-Malay indigenous people, and various other groups. The average age is 31.1 years, with a life expectancy at birth of 78 years. The population growth rate in Brunei Darussalam is 1.48% (Table 1).
Cancer Profile
Cancer has been the leading cause of death in Brunei Darussalam for over a decade.1,2 This is consistent with global trends today, wherein cancer is the leading cause of death before age 70 years in more than half of countries around the world.3 In Brunei Darussalam, the lifetime risk of being diagnosed with cancer is about one in four for men and one in three for women.4 The lifetime risk of cancer in Brunei Darussalam is much higher when compared with nearby countries, including neighboring Malaysia, which has a lifetime risk of 1 in 10 for men and 1 in 9 for women.5
Colorectal cancer has the highest incidence of all cancer types in Brunei Darussalam, with about 150 new cases recorded in 2020. The highest incidence of colorectal cancer is seen among men and women between the ages of 55 and 59 years. According to the National Cancer Registry in Brunei Darussalam, cases of advanced disease account for more than 70% of colorectal cancers in the country.2,4 The next most common cancers in Brunei Darussalam are breast cancer, lung cancer, stomach cancer, and cervical cancer (Figure 1).6
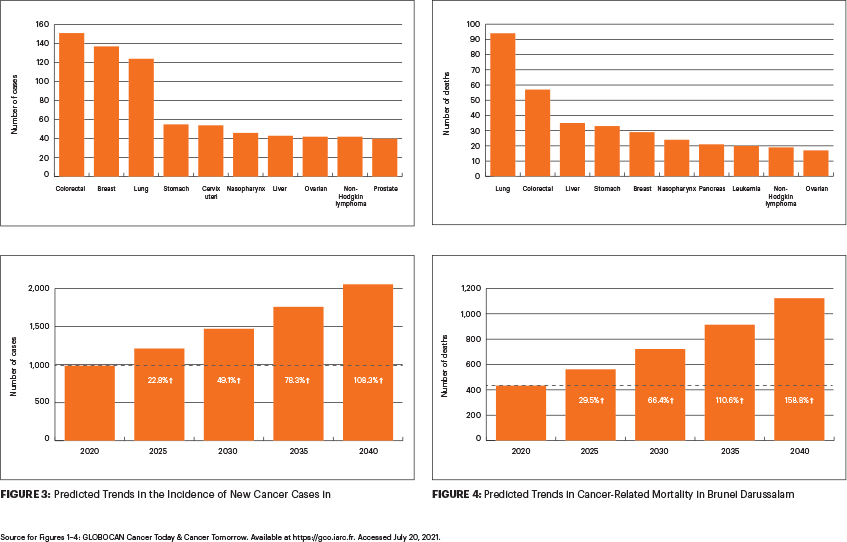
Globally, the most commonly diagnosed cancer is lung cancer.4 Though lung cancer is not the leading cancer by incidence in Brunei Darussalam, it does have the highest mortality, with 94 deaths due to lung cancer recorded in Brunei Darussalam in 2020 (Figure 2). The next most frequent causes of cancer-related mortality in Brunei Darussalam are colorectal cancer, liver cancer, stomach cancer, and breast cancer, with the number of deaths ranging from 57 to 29 deaths in 2020 (Figure 2).
In part due to population growth, increased life expectancy, and an aging population, the burden of cancer in Brunei Darussalam is expected to rise significantly in the years to come. Without effective intervention, the cancer incidence is predicted to increase more than 108% within the next 2 decades, from about 1,000 cancer cases in 2020 to more than 2,000 cancer cases in 2040 (Figure 3). During the same period, cancer deaths are predicted to rise even more—by almost 160%—from 434 cancer deaths in 2020 to 1,123 cancer deaths in 2040 (Figure 4).
Risk factors for colorectal cancer and other prevalent cancers in Brunei Darussalam include both modifiable factors (such as individual behaviors and habits) and nonmodifiable factors (such as genetic predispositions). About one in five adults is a current smoker, contributing to a high rate of cancer among adults in Brunei Darussalam, but this rate varies widely by gender; the prevalence of smoking in men is 36% compared with 4% among women.4 Nearly 14% of the population is obese, which, in combination with poor diet and physical inactivity, also contributes to the development of common cancers including colorectal cancer.7 Given the range of factors that influence cancer development, strategies to address a range of risk factors are needed.
Cancer Control Initiatives
Implementation of effective interventions, including those to reduce behavioral risk factors and increase early detection of cancer, may help curb the rising rates of cancer incidence and death in Brunei Darussalam. Several cancer prevention and control initiatives have already begun implementation; however, the success of national screening programs for early detection and control depends largely on the uptake of screening practices.
For example, a large, one-time screening program for colorectal cancer was conducted in Brunei Darussalam in 2009, as part of the National Integrated Health Screening program that ran from 2009 to 2013. The program used a single fecal immunochemical test for screening and found that only about 18% of patients referred attended a screening assessment. Of those who attended a screening session, only about half agreed to have a colonoscopy.2 Notably, all advanced lesions were detected in patients with a positive fecal immunochemical test. The program demonstrated that though uptake of colonoscopy screening was low, a single fecal test was effective for screening colorectal cancer.

Hope Craig, MSPH

Chandrakanth Are, MBBS, MBA, FSSO, FRCS, FACS
In 2011–2012, a national cervical cancer screening program was initiated in Brunei Darussalam and free human papillomavirus vaccination began being provided for adolescent girls.4 In 2019, Brunei Darussalam began implementing national cancer screening guidelines for breast cancer, cervical cancer, and colorectal cancer, as part of a larger national health screening program, to address the increasing incidence of noncommunicable diseases.8 The implementation of national screening programs for targeted cancers holds promise for improved early detection of high-risk cancers. To that end, the Brunei Ministry of Health is currently coordinating with other governmental and nongovernmental agencies to implement a national screening program.
Although health-care services are provided free of charge by the Brunei government, the current and predicted economic burdens of cancer in Brunei Darussalam are a concern for sustaining free health-care services.4 Cancer prevention and control initiatives, including strategies to increase comprehensive screening and reduce modifiable risk factors, are needed to enhance primary prevention and early detection and management of cancer.
Ms. Craig is Research Support Specialist at Cornell University, Ithaca, New York. Dr. Are is the Jerald L & Carolynn J. Varner Professor of Surgical Oncology & Global Health; Associate Dean for Graduate Medical Education; and Vice Chair of Education Department of Surgery, University of Nebraska Medical Center, Omaha.
DISCLOSURE: Ms. Craig reported no conflicts of interest. Dr. Are is a board member with Global Laparoscopy Solutions; has received research funding from Pfizer; and has a patent with the University of Nebraska Medical Center for a laparoscopy instrument.
REFERENCES
1. Brunei Darussalam Ministry of Health: Health Information Booklet 2016. Available at http:// www.moh.gov.bn/Downloadables/Health% 20Information%20Booklet%202016%20(21st%20Edition%20Revision%202).pdf. Accessed September 3, 2021.
2. Lim MA, Chong VH, Ong SK, et al: Colorectal cancer in Brunei Darussalam: An overview and rationale for national screening programme. Asian Pac J Cancer Prev 20:3571-3580, 2019.
3. World Health Organization: Cancer. Available at www.who.int/news-room/fact-sheets/detail/cancer. Accessed September 3, 2021.
4. Ong SK, Alikhan F, Lai DTC, et al: Population based lifetime risk estimation of malignant cancers in Brunei Darussalam. Brunei Int Med J 14:92-101, 2018.
5. National Cancer Institute, Malaysia Ministry of Health: Malaysian National Cancer Registry Report 2007–2011. Available at https:// www.crc.gov.my/wp-content/uploads/documents/report/MNCRRrepor2007-2011.pdf. Accessed September 3, 2021.
6. International Agency for Research on Cancer and World Health Organization: Globocan 2020. Available atgco.iarc.fr. Accessed July 13, 2021.
7. Central Intelligence Agency: The World Factbook—East Asia/Southeast Asia: Brunei. Available at https://www.cia.gov/the-world-factbook/countries/brunei. Accessed July 13, 2021.
8. Brunei Darussalam Ministry of Health: National Health Screening Guideline on Noncommunicable Diseases. Available at http://www.moh.gov.bn/Shared%20Documents/MOH_National%20Health%20Screening%20Guideline%20on%20NCDs_23%20Jul%202020.pdf. Accessed September 3, 2021.

