In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
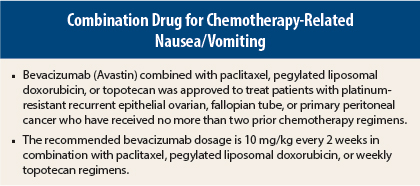
On November 14, 2014, bevacizumab (Avastin) in combination with paclitaxel, pegylated liposomal doxorubicin, or topotecan was approved for treatment of patients with platinum-resistant recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who have received no more than two prior chemotherapy regimens.1,2
Supporting Trial
Approval was based on the finding of prolonged progression-free survival in the international open-label phase III AURELIA trial, in which 361 patients with platinum-resistant disease were randomly assigned to receive bevacizumab plus chemotherapy (n =179) or chemotherapy alone (n = 182).2,3 Chemotherapy consisted of paclitaxel (80 mg/m2 on days 1, 8, 15, and 22 every 4 weeks), pegylated liposomal doxorubicin (40 mg/m2 on day 1 every 4 weeks), or topotecan (4 mg/m2 on days 1, 8, and 15 every 4 weeks or 1.25 mg/m2 on days 1 to 5 every 3 weeks). Bevacizumab was given at 10 mg/kg every 2 weeks or at 15 mg/kg every 3 weeks in patients receiving topotecan in the 3-week schedule. Investigator-assessed progression-free survival was the primary endpoint.
Patients had received no more than two prior chemotherapy regimens and had experienced a recurrence at no more than 6 months from the most recent platinum-based therapy. Patients with evidence of rectosigmoid involvement by pelvic examination, bowel involvement on computed tomography scan, or clinical symptoms of bowel obstruction were excluded.
Overall, patients had a median age of 61 years (range = 25–84 years; 37% ≥ 65 years), 79% had measurable disease; 87% had CA-125 level at least 2 × upper limit of normal; 31% had ascites; platinum-free interval was 3 to 6 months in 73% and < 3 months in 27%; and Eastern Cooperative Oncology Group performance status was 0 in 59%, 1 in 34%, and 2 in 7%.
Among all patients, median progression-free survival was 6.8 months with bevacizumab/chemotherapy vs 3.4 months with chemotherapy (hazard ratio [HR] = 0.38, P < .0001, stratified log-rank test). Median overall survival did not significantly differ between groups (16.3 vs 13.3 months, HR = 0.89, 95% confidence interval [CI] = 0.69–1.14). Objective response rate was 28% vs 13%, and median duration of response was 9.4 vs 5.4 months.
Exploratory analyses by chemotherapy regimen showed that the best outcomes were for the bevacizumab/paclitaxel vs paclitaxel comparison (n = 60 vs 55), with median progression-free survival of 9.6 vs 3.9 months (HR = 0.47, 95% CI = 0.31–0.72), median overall survival of 22.4 vs 13.2 months (HR = 0.64, 95% CI = 0.41–1.01), and response rate of 53% vs 30%. This analysis suggests that patients with prior paclitaxel treatment may benefit from bevacizumab plus weekly paclitaxel.
For the bevacizumab/pegylated liposomal doxorubicin vs doxorubicin comparison (n = 62 vs 64), median progression-free survival was 5.1 vs 3.5 months (HR = 0.47, 95% CI = 0.32–0.71), median overall survival was 13.7 vs 14.1 months (HR = 0.94, 95% CI = 0.63–1.42), and objective response rate was 16% vs 8%.
For the bevacizumab/topotecan vs topotecan comparison (n = 57 vs 63), median progression-free survival was 6.2 vs 2.1 months (HR = 0.24, 95% CI = 0.15–0.38), median overall survival was 13.8 vs 13.3 months (HR = 1.12, 95% CI = 0.73–1.73), and response rate was 17% vs 2%.
How It Works
Bevacizumab is recombinant humanized monoclonal IgG1 antibody that binds vascular endothelial growth factor (VEGF) and prevents interaction of VEGF with its receptors on the surface of endothelial cells. Inhibition of this interaction results in inhibition of endothelial cell proliferation and new blood vessel formation in in vitro models of angiogenesis.
How It Is Given
The recommended bevacizumab dosage is 10 mg/kg every 2 weeks in combination with paclitaxel, pegylated liposomal doxorubicin, or weekly topotecan regimens. Bevacizumab at 15 mg/kg every 3 weeks may be combined with topotecan regimen given every 3 weeks. The chemotherapy regimens are paclitaxel at 80 mg/m2 on days 1, 8, 15, and 22 every 4 weeks; pegylated liposomal doxorubicin at 40 mg/m2 on day 1 every 4 weeks; or topotecan at 4 mg/m2 on days 1, 8, and 15 every 4 weeks or at 1.25 m/m2 on days 1 to 5 every 3 weeks.
There are no recommended dose reductions for bevacizumab. Treatment should be permanently discontinued for gastrointestinal (GI) perforations (GI perforations, fistula formation in the GI tract, intra-abdominal abscess) or fistula formation involving an internal organ; wound dehiscence and wound healing complications requiring medical intervention; serious hemorrhage; severe arterial thromboembolic events; life-threatening (grade 4) venous thromboembolic events, including pulmonary embolism; hypertensive crisis or hypertensive encephalopathy; posterior reversible encephalopathy syndrome; or nephrotic syndrome.
Bevacizumab should be temporarily suspended at least 4 weeks prior to elective surgery and for severe hypertension not controlled with medical management, moderate to severe proteinuria, and severe infusion reactions. Bevacizumab should not be given to patients with serious hemorrhage or recent hemoptysis.
Safety Profile
In the phase III trial, grade 2 to 4 adverse events occurring at an incidence ≥ 5% higher in the bevacizumab/chemotherapy group included neutropenia (30.7% vs 25.4%), hypertension (19.0% vs 5.5%), peripheral sensory neuropathy (17.9% vs 7.2%), mucosal inflammation (12.8% vs 5.5%), and proteinuria (12.3% vs 0.6%). Grade 3 or 4 adverse events occurring at an incidence ≥ 2% higher consisted of hypertension (6.7% vs 1.1%) and palmar-plantar erythrodysesthesia syndrome (4.5% vs 1.7%). GI perforation occurred in 1.7% of bevacizumab-treated patients.
The exclusion of patients with evidence of rectosigmoid involvement, bowel involvement, or bowel obstruction from this trial may have contributed to the relatively low rate of perforation observed. Fistulae occurred in 2% of bevacizumab-treated patients and in no patients receiving chemotherapy alone.
Bevacizumab carries boxed warnings for GI perforation, surgery and wound healing complications, and hemorrhage (including severe or fatal hemorrhage, hemoptysis, gastrointestinal bleeding, central nervous system [CNS] hemorrhage, and vaginal bleeding). The appropriate interval between termination of bevacizumab and subsequent elective surgery to reduce the risk of impaired wound healing/wound dehiscence has not been determined; in addition to discontinuing bevacizumab ≥ 28 days prior to elective surgery, it should not be restarted for ≥ 28 days after surgery and until the surgical wound is fully healed.
Severe or fatal hemorrhage, including hemoptysis, GI bleeding, CNS hemorrhage, epistaxis, and vaginal bleeding, occur up to fivefold more frequently in patients receiving bevacizumab.
Bevacizumab also carries warnings/precautions for perforation or fistula, arterial thromboembolic events, venous thromboembolic events, hypertension, posterior reversible encephalopathy syndrome, proteinuria, infusion reactions, and ovarian failure. Patients must undergo routine monitoring of blood pressure and urine protein. Women of reproductive potential must be informed of the risk of ovarian failure. ■
References
1. U.S. Food and Drug Administration: Bevacizumab solution. Available at www.fda.gov.
2. AVASTIN® (bevacizumab) solution for intravenous infusion prescribing information, Genentech, Inc, November 2014. Available at www.accessdata.fda.gov.
3. Pujade-Lauraine E, Hilpert F, Weber B, et al: Bevacizumab combined with chemotherapy for platinum-resistant recurrent ovarian cancer. J Clin Oncol 32:1302-1308, 2014.