The androgen receptor inhibitor enzalutamide (Xtandi) showed encouraging activity as a single agent in advanced triple-negative breast cancer patients expressing the androgen receptor, according to an international study presented at the 2014 San Antonio Breast Cancer Symposium.1
Enzalutamide directly binds to the androgen receptor and is a potent inhibitor of signaling. It is approved in metastatic castration-resistant prostate cancer.
Clifford A. Hudis, MD, FACP, of Memorial Sloan Kettering Cancer Center, New York, one of the study’s investigators, commented on the findings from this study and the drug’s potential in this subset of patients.
“We have been pursuing the role of androgen receptor inhibitors for years, after discovering that a small percentage of [patients with triple-negative disease], who historically have not been responsive to hormone therapy, express the androgen receptor,” he said.
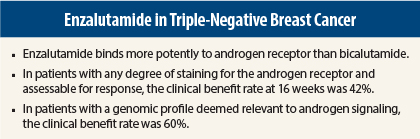
Enzalutamide is “a more modern, more potent agent” than bicalutamide—having eight times higher affinity for the receptor. Bicalutamide is approved in prostate cancer and has shown some activity in breast cancer as well.2
“We have now asked whether enzalutamide is active in breast cancer, and in the era of precision medicine, this study really resonates,” Dr. Hudis said.
“While this is a small subset—20% to 40% of the triple-negative subtype, which is a modest percentage of all breast cancers—we saw that enzalutamide as a single agent can be given to these patients, whose standard treatment is chemotherapy, and yield meaningful palliation and even RECIST responses, with modest and limited toxicities.”
Two-Stage Study Design
The study screened 404 patients with advanced triple-negative breast cancer and enrolled 118 shown to express the androgen receptor (androgen receptor–positive > 0% staining; androgen receptor–negative = 0% staining). Patients were treated with single-agent enzalutamide at 160 mg daily until disease progression. The primary endpoint was clinical benefit rate at 16 weeks in evaluable patients—ie, those with androgen receptor staining in ≥ 10% of tumor and at least one postbaseline tumor assessment.
Stage 1 of the study included 42 patients; the study required that at least 3 of 26 evaluable patients obtain clinical benefit, (ie, complete response, partial response, or stable disease) in order to be expanded to stage 2. In stage 2 (n = 76), at least 9 of 62 evaluable patients must meet the endpoint, for the null hypothesis to be rejected.
In the current analysis of the stage 1 patients, single-agent enzalutamide demonstrated strong antitumor activity, with a clinical benefit rate at 16 weeks of 42% in 26 evaluable patients (24% in the intent-to-treat population). Of these, 82% also maintained clinical benefit at 24 weeks.
In addition, “the first objective responses from anti–androgen receptor therapy were observed with enzalutamide,” reported Tiffany A. Traina, MD, of Memorial Sloan Kettering Cancer Center, who was the study’s first author.
Two patients in stage 1 had a complete or partial response. In stage 2, one additional patient to date has achieved a complete response, and three have achieved a partial response.
Pointing to CT scan images on the poster from a patient treated at Memorial Sloan Kettering, Dr. Traina said, “She had a clear, confirmed response after visceral metastases and multiple sites of disease. It was a real-deal response, and she is still on therapy.”
Novel Diagnostic Assay
“It may be possible to identify patients who benefit from enzalutamide,” Dr. Traina indicated. A novel genomic-based biomarker was tested [not further described], and investigators concluded “it may be superior to immunohistochemistry.”
In diagnostic-positive patients, median progression-free survival was 2.5 times greater than for diagnostic-negative patients (20 vs 8 weeks) and the clinical benefit rate at 24 weeks in diagnostic-positive patients (42%–60%) parallels that of hormonal agents in hormone receptor–positive disease, the investigators reported.
Approximately 50% of the intent-to-treat population was diagnostic-positive by this methodology. Work is ongoing to confirm these findings in the stage 2 population.
Dr. Traina added that for the population with a positive diagnostic profile and treated in the first or second line, the clinical benefit rate at 24 weeks was 60%. “This is phenomenal for a hormonal agent in triple-negative breast cancer,” she indicated.
Enzalutamide was well tolerated. Toxicities were primarily mild-to-moderate fatigue and gastrointestinal symptoms, and appeared similar to other hormonal therapies for breast cancer. Seven percent of patients discontinued treatment due to an adverse event.
This is the largest prospective clinical study conducted in patients with androgen receptor–positive triple-negative breast cancer. Mature data from all 118 patients are expected in 2015. ■
Disclosure: Dr. Traina reported that she is a consultant for Genentech, Eisai, Halozyme, Celgene, and Prostrakan and has received research support from Medivation, AstraZeneca, Eisai, Janssen, Genentech, and Novartis. Dr. Hudis reported no potential conflicts of interest.
References
1. Traina TA, et al: San Antonio Breast Cancer Symposium. Abstract P5-19-09. Presented December 12, 2014.
2. Gucalp A, et al: Clin Cancer Res 19:5505-5512, 2012.