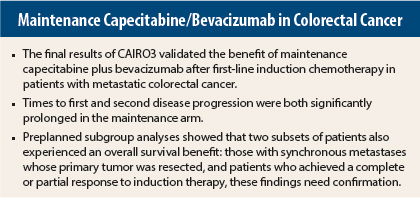
In patients with metastatic colorectal cancer, maintenance treatment with capecitabine plus bevacizumab (Avastin) after induction treatment with capecitabine, oxaliplatin, and bevacizumab (CAPOX-B) significantly delayed disease progression, compared to observation, according to the final results of the phase III CAIRO3 trial by the Dutch Colorectal Cancer Group.1 This benefit was evident across all subgroups of patients. The findings were reported at the 2014 Gastrointestinal Cancers Symposium in San Francisco.
The investigators also found a nonsignificant benefit in the secondary endpoint of overall survival. Preplanned subgroup analysis showed that this overall survival benefit was restricted to patients with synchronous disease who had their primary tumor resected and patients with complete or partial response as best response on induction treatment. However, these latter findings require further confirmation.
Maintenance treatment with capecitabine plus bevacizumab after six cycles of CAPOX-B significantly prolonged the time to first disease progression, and also the time from randomization to progression after reintroduction of CAPOX-B (ie, second progression), which was the study’s primary endpoint, according to Miriam Koopman, MD, PhD, of University Medical Center Utrecht in the Netherlands.
“Preplanned subgroup analyses showed the benefit of maintenance treatment in all subgroups for the primary endpoint, and an overall survival benefit for maintenance treatment in patients with synchronous disease with resection of the primary tumor, and in patients with a complete or partial response as best response on induction treatment,” she said.
Study Details
To help define the optimal duration of chemotherapy and bevacizumab in metastatic colorectal cancer, CAIRO3 evaluated the efficacy of maintenance with capecitabine plus bevacizumab vs observation in patients who had not had disease progression during induction treatment with CAPOX-B. Of note, patients in whom a radical resection of metastases was planned were also excluded from the study.
The 558 patients with previously untreated metastatic colorectal cancer enrolled in CAIRO3 achieved a response or stable disease after six cycles of CAPOX-B, then were randomly assigned to continue on maintenance capecitabine plus bevacizumab or to undergo observation. The maintenance regimen was capecitabine at 625 mg/m2 twice daily, given continuously with bevacizumab at 7.5 mg/kg every 3 weeks.
Upon first progression, patients in both arms were scheduled to receive CAPOX-B until second progression, which was the primary endpoint. After a median follow-up of 48 months, CAPOX-B was reintroduced to 61% of the observation arm, compared to 47% of the maintenance arm.
The median first episode of disease progression (PFS1) was 4.1 months in the observation arm and 8.5 months in the maintenance arm, a 57% reduction in risk of progression (P < .0001). Median time to second progression (PFS2), the primary endpoint, was 8.5 months vs 11.7 months, respectively, a 33% reduction in risk (P < .0001), Dr. Koopman reported.
She emphasized that the time to all endpoints was assessed from randomization and did not include the 4 to 5 months of induction treatment. She also noted that PFS2 was considered equal to PFS1 for patients in whom CAPOX-B was not reintroduced after first progression for any reason.
Another endpoint, the time to second progression of disease (TT2PD) included patients who received any treatment after first progression, including CAPOX-B. The clinical relevance of this endpoint was explained by the fact that a substantial number of patients were not able or willing to receive reinduction treatment of CAPOX-B upon PFS1. Median TT2PD was 11.1 months with observation and 13.9 months with maintenance, a 32% reduction in risk with maintenance (P < .0001).
Median overall survival was 18.1 months with observation and 21.6 months with maintenance, which was not a significant difference (hazard ratio = 0.89; P = .22).
The drugs administered during metastatic disease were not significantly different between the arms, with about half the patients in each arm receiving a total of four drugs and 12% receiving five.
“Quality of life was maintained during maintenance treatment, and was clinically not inferior compared to the quality of life in the observation arm,” Dr. Koopman noted.
Interesting Subgroup Differences
The benefit of maintenance was present in all subgroups for the primary endpoint (PFS2), as well as for PFS1 and TT2PD, but some interesting treatment interactions emerged upon deeper analysis.
Multivariable analysis for overall survival, with treatment adjusted for a series of potentially confounding factors at baseline, showed significant interactions for treatment (observation vs maintenance) with resection of the primary tumor (yes vs no) and synchronous vs metachronous metastases at baseline (P < .0001 for both interactions), Dr. Koopman reported.
The greatest benefit was observed for the 180 patients with synchronous metastases whose primary tumors were resected. With maintenance, these patients achieved a median overall survival of 25 months, vs 18 months with observation (P < .0001). For the 230 patients with synchronous metastases and no resection of the primary tumor, median overall survival was 16.3 months with observation and 14.9 months with maintenance, she reported.
Patients who achieved a complete or partial response on induction treatment before randomization also had very favorable median overall survival with maintenance—24.1 months vs 18.8 months with observation (P < .0001).
Given the fact that these subgroup analyses concerned a secondary endpoint, Dr. Koopman stressed that these findings require further confirmation. The main outcome of the CAIRO3 study is that patients with metastatic colorectal cancer receiving induction treatment with CAPOX-B do benefit from maintenance treatment with capecitabine plus bevacizumab. ■
Disclosure: Dr. Koopman reported an advisory role for Amgen, Bayer, Merck-Serono, and Roche.
Reference
1. Koopman M, Simkens L, May A, et al: Final results and subgroup analyses of the phase 3 CAIRO3 study: Maintenance treatment with capecitabine plus bevacizumab versus observation after induction treatment with chemotherapy plus bevacizumab in metastatic colorectal cancer. 2014 Gastrointestinal Cancers Symposium. Abstract LBA388. Presented January 18, 2014.