 Susan O’Brien, MD, Professor in the Department of Leukemia at The University of Texas MD Anderson Cancer Center, Houston, has a special interest in novel developments in the treatment of acute lymphoblastic leukemia (ALL). At the 2011 ASH Annual Meeting, she discussed her picks of top newsmakers in this tumor type.
Susan O’Brien, MD, Professor in the Department of Leukemia at The University of Texas MD Anderson Cancer Center, Houston, has a special interest in novel developments in the treatment of acute lymphoblastic leukemia (ALL). At the 2011 ASH Annual Meeting, she discussed her picks of top newsmakers in this tumor type.
Moxetumomab
“A number of monoclonal antibodies being reported here at ASH look very interesting,” said Dr. O’Brien. She first mentioned moxetumomab, a CD22 antibody conjugated with the Pseudomonas exotoxin. Moxetumomab is being investigated in a phase I study in pediatric patients with relapsed/refractory ALL.1
“They have not reached a maximum tolerated dose yet, but even without that they report about a 30% response rate in a very heavily pretreated population. And remember,” she emphasized, “ALL is not like [chronic lymphocytic leukemia], or a low-grade lymphoma, where we treat patients, and if they relapse we treat them again until we gain a lasting response. With ALL, we use all of our effective agents upfront so that when patients relapse, we do not have several unused agents still to try.”
Inotuzumab Ozogamicin
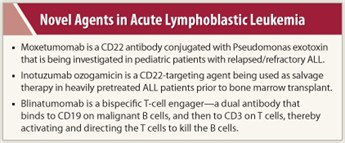 A second agent for ALL on Dr. O’Brien’s radar was inotuzumab ozogamicin, a CD22-targeting agent that is conjugated to the same toxin, ozogamicin, as the acute myeloid leukemia drug gemtuzumab ozogamicin (Mylotarg). “This is the same toxin with a different antibody,” she explained, “except in this case we are targeting CD22, a cell-surface molecule present in over 90% of patients with ALL.”
A second agent for ALL on Dr. O’Brien’s radar was inotuzumab ozogamicin, a CD22-targeting agent that is conjugated to the same toxin, ozogamicin, as the acute myeloid leukemia drug gemtuzumab ozogamicin (Mylotarg). “This is the same toxin with a different antibody,” she explained, “except in this case we are targeting CD22, a cell-surface molecule present in over 90% of patients with ALL.”
As reported by Kebriaei et al, inotuzumab ozogamicin was used as salvage therapy in a small study of 19 heavily pretreated ALL patients prior to bone marrow transplant.2 With a follow-up of 3 months among surviving patients, both overall and progression-free survival rates were 59%. This response allowed for more patients to proceed to successful transplant than would have been historically expected with standard treatment. Of the 19 subjects, 10 had minimal residual disease at time of the procedure.
Those 19 patients were actually a subset of a larger group reported by Dr. O’Brien at the ASH meeting.3 Among all 49 patients with refractory or relapsed CD22-positive ALL, the overall response rate was 57%—the highest response rate reported for single-agent therapy in adult ALL. Median survival for the whole population was 5 months.
Blinatumomab
Dr. O’Brien is also keenly interested in blinatumomab, an agent in the so-called BiTE [bispecific T-cell engager] antibody drug class. “It’s a dual antibody that first binds to CD19 on malignant B cells, and then binds to CD3 on nearby T cells, thereby activating the T cells and directing them to kill the B cells,” she explained.
Success with this agent was recently reported in the Journal of Clinical Oncology.4 “That was a minimal residual disease study that showed the ability to convert 16 of 21 chemotherapy-refractory patients to [minimal residual disease] negativity, and it appeared to be very durable,” she recalled. The probability for relapse-free survival was 78% at a median follow-up of 405 days.
At the ASH meeting, investigators reported on a cohort of 18 ALL patients in full-blown relapse who received single-agent blinatumomab, 12 of whom achieved a complete remission within two cycles, corresponding to a response rate of 67%.5 Of these 12 responding patients, 75% had complete hematologic recovery of peripheral blood counts.
Dr. O’Brien was impressed with blinatummab specifically, and the new drug class in general, commenting that “these dual antibodies are very hot in ALL.”■
Disclosure: Dr. O’Brien reported no potential conflicts of interest.
References
1. Wayne AS, Bhojwani D, Silverman LB, et al: A novel anti-CD22 immunotoxin, moxetumomab pasudotox: A phase I study in pediatric acute lymphoblastic leukemia. 53rd American Society of Hematology Annual Meeting. Abstract 248. Presented December 12, 2011.
2. Kebriaei P, Wilhelm K, Ravandi F, et al: Inotuzumab ozogamicin is an effective salvage therapy that allows for allogeneic hematopoietic stem cell transplantation in remission in patients with advanced acute lymphoblastic leukemia. 53rd American Society of Hematology Annual Meeting. Abstract 3102. Presented December 11, 2011.
3. O’Brien S, Thomas DA, Ohanian M, et al: Inotuzumab ozogamycin (I0), a CD22 monoclonal antibody conjugated to calecheamicin, is active in refractory-relapse acute lymphocytic leukemia (R-R ALL). 53rd American Society of Hematology Annual Meeting. Abstract 875. Presented December 12, 2011.
4. Topp MS, Kufer P, Goekbuget N, et al: Targeted therapy with the T-cell–engaging antibody blinatumomab of chemotherapy-refractory minimal residual disease in B-lineage acute lymphoblastic leukemia patients results in high response rate and prolonged leukemia-free survival. J Clin Oncol 29:2493-2498, 2011.
5. Topp MS, Goekbuget N, Zugmaier G, et al: Anti-CD19 BiTE blinatumumab induces high complete remission rate in adult patients with relapsed B-precursor ALL: Updated results of an ongoing phase II trial. 53rd American Society of Hematology Annual Meeting. Abstract 252. Presented December 12, 2011.

