Limited-stage nonbulky diffuse large B-cell lymphoma (DLBCL) carries an excellent prognosis, and radiotherapy provides no value in patients who obtain a complete response, according to the phase III 02-03 trial from the Lysa/Goelams group, presented at the 56th American Society of Hematology (ASH) Annual Meeting and Exposition.1
“The benefit of radiotherapy following chemotherapy in limited-stage DLBCL remains controversial. Before the ‘rituximab [Rituxan] era,’ four randomized trials turned in conflicting results. More recently, the German Unfolder study prematurely closed the R-CHOP without radiotherapy arm in bulky limited-stage DLBCL due to an excess of relapse,” said Thierry Lamy, MD, PhD, of the University Hospital of Rennes in France.
To further examine the benefit of radiotherapy after R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) in this population, Dr. Lamy and colleagues initiated a randomized trial in patients with nonbulky (tumor size < 7 cm) limited-stage DLBCL in 2005.
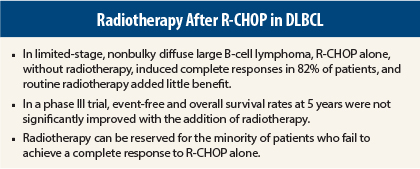
They concluded that radiotherapy following R-CHOP is of no value to the vast majority of patients.
“With the current follow-up, the addition of radiotherapy is not significantly superior to R-CHOP alone and should be reserved for the minority of patients who do not reach complete response after R-CHOP,” Dr. Lamy said.
Study Details
Depending on risk factors, patients received 4 or 6 consecutive cycles of R-CHOP14, followed or not by involved-field radiotherapy at 40 Gy delivered 4 weeks after the last cycle of R-CHOP. All patients were evaluated by fluorodeoxyglucose–positron emission tomography (FDG-PET) at baseline, after 4 cycles of R-CHOP, and at the end of treatment.
The recommendation was that patients in partial response (tumor regression > 50% but a persistent positive FDG-PET) after cycle 4 receive an additional 2 cycles of R-CHOP followed by radiotherapy. The primary objective was event-free survival 1 year after the last randomization.
There were 301 evaluable patients (median age, 56 years), of whom 82% had normal LDH levels, 96% had no B symptoms, and the majority had an International Prognostic Index score of 1 to 2. The main tumor site was cervical lymph nodes, and 40% had extranodal sites.
No Additional Benefit of Radiotherapy
No significant benefit was observed in the cohort receiving radiotherapy after R-CHOP (n = 151) compared with the group receiving R-CHOP alone (n = 150). Complete response rates overall were 84%, and 14% of patients attained partial responses and three patients had stable disease.
In the intent-to-treat analysis, after 51 months’ median follow-up, event-free survival at 5 years was 88%, with 88.4% for the radiotherapy arm and 87.3% for the R-CHOP alone arm (P = .13). Overall survival was 91% for the whole population and 92% for the radiotherapy arm and 90% for the R-CHOP–alone arm (P = .33), Dr. Lamy reported.
By assignment group, complete responses were observed in 82% after R-CHOP alone and 85% after R-CHOP plus radiotherapy; partial responses (PET-positive) were observed in 16% and 12%, and stable disease was noted in one and two patients, respectively.
At the end of treatment, complete responses were observed in 93% and 95%, respectively. There were partial responses in seven patients treated with R-CHOP alone and one patient treated with R-CHOP plus radiotherapy, and stable disease was reported in two patients in the R-CHOP arm, Dr. Lamy added.
For the 43 patients who were partial responders after cycle 4, 37 (86%) received 2 additional cycles of R-CHOP plus radiotherapy, whereas 6 patients were treated with a different regimen, with or without radiotherapy. Of these 43 patients, 40 ultimately attained a complete response. After complete response, 5-year event-free survival was 89% in the R-CHOP–alone arm, and 91% in the R-CHOP plus radiotherapy arm.
“After 4 cycles of R-CHOP, adding 2 cycles plus radiotherapy for patients in partial response induced similar outcomes as compared to patients who obtained a complete response,” Dr. Lamy pointed out.
Relapses occurred in 12 patients (8%) in the R-CHOP–alone arm and 8 patients (5%) of the arm receiving R-CHOP plus radiotherapy, which was not a significant difference. The median time to relapse was 21 months. In the radiotherapy arm, none of these relapses occurred at the initial tumor site, but in the R-CHOP–alone arm, 5 of 12 relapses occurred at that site. Altogether, nine patients developed progressive disease.
“In this prospective study, the results demonstrate that in nonbulky limited-stage DLBCL, R-CHOP alone for 4 to 6 cycles induces very high complete response rates, with a very good overall survival and a very low relapse rate,” he concluded. ■
Disclosure: Dr. Lamy reported no potential conflicts of interest.
Reference
1. Lamy T, Damaj G, Gyan E, et al: R-CHOP with or without radiotherapy in non-bulky limited-stage diffuse large B cell lymphoma (DLBCL): Preliminary results of the prospective randomized phase III 02-03 trial from the Lysa/Goelams Group. 2014 ASH Annual Meeting. Abstract 393. Presented December 8, 2014.