Mammograms often miss occult breast cancers concealed in dense breasts. Women with dense breasts represent about 40% to 50% of women who undergo mammography screening. In some states and centers in the United States, women with dense breasts are routinely offered ultrasonography following a negative mammography, and four states have laws including a phrase regarding the availability of “supplemental screening options, that may include ultrasound or magnetic resonance imaging [MRI]” for these women. Laws enacted in 19 states require that radiologists notify patients of their breast density in the “lay letter” that provides screening mammography results. Moreover, four states have mandatory insurance coverage of supplemental breast ultrasound screening, although two of those four states do not yet have notification laws.
A large, retrospective, “real-world” study from five different radiology sites that are part of the Hospital of Central Connecticut confirmed that screening breast ultrasonography detects occult malignancy in women with dense breasts and that these cancers were not detected by mammography.1 Women with dense breasts were offered ultrasonography after negative mammography screening.
Data from 4 years of screening ultrasound were retrospectively reviewed, after Connecticut passed the first law that mandated informing patients whether or not they have dense breast tissue on mammogram and that mammography may miss some cancers.
“We may need a new paradigm for screening. We have to deal with risk assessment in a simpler way. Low-risk women with no dense breast tissue should get mammography beginning at age 40. Women with a 25% or greater risk of breast cancer should get mammography and magnetic resonance imaging (MRI). Middle-of-the-road women with dense breast tissue and maybe one or two family members with breast cancer should be offered screening mammography and ultrasonography for early detection of breast cancer,” said lead author Jean M. Weigert, MD, of the Hospitals of Central Connecticut, New Britain, Connecticut.
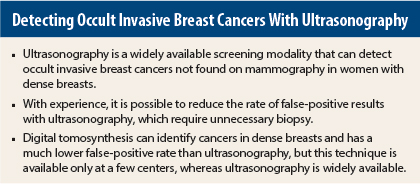
Noting that digital tomosynthesis could be a big improvement over ultrasonography for detecting occult cancers, she said it would not be readily available to a majority of women for a number of years. “I’m from the real world, where everyone has ultrasound.”
Positive Predictive Value Increased Over Time
About 31,000 mammograms were performed each year, and about 3,000 ultrasonographic exams were performed each year in women with dense breasts. The numbers of cancers detected per 1,000 women remained constant throughout the study. In year 1, 2,706 women underwent breast ultrasonography for dense breasts, and 11 cancers were detected. In year 4, 3,331 women were offered ultrasonography, and 11 cancers were detected.
“Over time and with experience, we were able to identify lesions that needed to be biopsied,” said Dr. Weigert. Since false-positives are a downside of both mammography and ultrasonography, this is good news, she said, in an interview with The ASCO Post. When she reviewed the first 2 years and the last 2 years separately, the numbers of biopsies dropped with experience, yet the cancer detection rate remained the same.
“We found all types and grades of cancers, including lobular, invasive ductal, combined ductal carcinoma in situ and lobular, ductal carcinoma in situ, and also atypical hyperplasia, which is a risk factor for breast cancer. They were predominantly estrogen receptor–positive and progesterone receptor–positive breast cancers in these women, with very few risk factors other than dense breast tissue. They are exactly the kinds of cancers we hope to find on mammography, but it took ultrasonography to find them,” she stated.
Because many of the same patients were coming in for yearly screening, the cancers detected in year 4 were smaller, she added. By year 4, most of the detected lesions were smaller than 1 cm, with no sentinel lymph node involvement.
Although ultrasonography would add to the cost of screening, “there is no free lunch,” Dr. Weigert said. “Finding a cancer that is easier to treat would certainly have the potential to reduce costs of treating a more advanced cancer,” she stated.
Academic Center Perspective
Discussant of this study, Jafi A. Lipson, MD, of Stanford University School of Medicine, Palo Alto, California, reviewed Dr. Weigert’s study from the perspective of experience at a radiology center with the latest technology—digital tomosynthesis (three-dimensional digital mammography)—which is currently not widely available in community centers.
“Density is a qualitative assessment that we make on the basis of a mammogram. There are four types of density, and density is an independent risk factor for breast cancer,” she said. “Density reduces the sensitivity of mammography and masks cancers, driving the search for a better modality to detect these cancers.”
Breast cancer advocacy groups have been working toward having radiologists report breast density as part of screening information, and 20 states now have notification laws. Insurance coverage for supplemental screening of dense breasts is mandated in four states in the United States, and federal legislation is pending, Dr. Lipson said.
Supplemental screening options include MRI for women who have more than a 25% lifetime risk of developing breast cancer, digital tomosynthesis, and ultrasonography. “All of these modalities have a range of benefits and harms. The benefit-to-harm ratio is determined by the prior probability of disease and the value placed on increased cancer detection given the risk of false-positive exams,” she said.
Dr. Lipson agreed that ultrasonography can detect mammographically occult cancers, but she had several issues with this study. “Because of the lack of a control group and no long-term follow-up, the true clinical impact of finding these cancers is unknown. It is not known if these cancers would have been detected by the next mammography screening. Also, the impact on mortality is unknown.”
Turning to the harms of screening, she said that ultrasonography has a much higher rate of false-positives than mammography and digital tomosynthesis. “Many more biopsies are generated by screening ultrasonography than mammography, and most are false-positives,” she stated.
Cost Considerations
A recent study found that 4 breast cancer deaths would be averted for every 10,000 women screened by ultrasonography and that 1.7 quality-adjusted life years would be gained with ultrasonographic screening of women with dense breasts.2 Ultrasonography would lead to 354 biopsies for false-positive results per 1,000 women compared with mammography. The cost per year of quality-adjusted life years gained would be $325,000, and assuming a threshold of $50,000 to $60,000 per quality-adjusted life year, would not be considered cost-effective, she noted. When only women with extremely dense breasts were considered, the cost per quality-adjusted life year gained would be $246,000, which is still unacceptable.
“These authors concluded that ultrasonography substantially increases costs while producing only small benefits,” she stated.
Challenge of Filtering the Data
“By contrast, digital tomosynthesis reduces false-positives by 15% to 30% and increases cancer detection by 30% to 50%, according to multiple prospective national and international studies,”3 Dr. Lipson continued.
Currently, there are no published head-to-head studies comparing supplemental screening ultrasonography vs digital tomosynthesis. Both technologies increase the rate of cancer detection, but the false-positive rate is about four times greater with ultrasound than with mammography and 30% to 40% lower with tomosynthesis, she said.
“It can be challenging for women and their physicians to filter all of this information. There are now multiple new screening technologies, with no long-term outcome data regarding their true clinical impact. Most states with notification laws do not have insurance for these tests,” she said.
She directed listeners to www.breastdensity.info for more information on this issue. This website is not beholden to any commercial sponsor and is a joint effort created by a working group of breast radiologists and breast cancer risk specialists, representing academic and community-based practices across California, formed to assist patients, referring doctors, and radiologists in responding to new legislation mandating that radiologists report breast density to patients. ■
Disclosure: Dr. Weigert is a consultant for Tractus Inc. Dr. Lipson reported no potential conflicts of interest.
References
1. Weigert JM: The Connecticut experiment: 4 years of screening women with dense breasts with bilateral ultrasound. 2014 San Antonio Breast Cancer Symposium. Abstract S5-01. Presented December 12, 2014.
2. Sprague BL, Stout NK, Schechter C, et al: Benefits, harms, and cost-effectiveness of supplemental ultrasonography screening for women with dense breasts. Ann Intern Med. December 9, 2014 (early release online).
3. Friedewald SM, Rafferty EA, Rose SL, et al: Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA 311:2499-2507, 2014.