Diagnosed with stage IV non–small cell lung cancer in 2011, Stephen Wright turned to patient support groups where he learned about the anaplastic lymphoma kinase (ALK) mutation and a new drug that targeted it, crizotinib (Xalkori). He asked—then insisted—that he be tested for the mutation. He found he was ALK-positive. He subsequently spent 4 hours on the phone convincing his insurance company to cover the drug, which had just been approved by the U.S. Food and Drug Administration.
Two and a half years later, Stephen chased his children up and down the National Mall in Washington while waiting to attend Rev 2014, a forum focused on navigating cancer in the era of personalized medicine. For the oncologists, nurses, pathologists, patient advocates, and others gathered across from the Mall, his story encapsulated many of the issues they were there to talk about.
Stephen is not the only one, said Bradley Ozenberger, PhD, of The Genome Institute at Washington University in an opening talk. Occasionally, other patients with advanced cancer have had the luck to find and benefit from a new targeted drug. “But how do we make the leap to have it work for everyone?” he asked.
Answers to that question over the next 2 days ranged from greater patient engagement with their own diagnosis and treatment, to a new understanding of quality of care that incorporates personalized medicine, to better access to data, including good and timely information for providers, pathologists, and patients about biomarkers, targeted drugs, and their companion diagnostics.
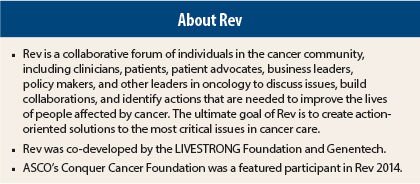
Convened by the LIVESTRONG Foundation and Genentech, and with ASCO’s Conquer Cancer Foundation a featured participant, Rev 2014 (see sidebar below) was designed to generate new ideas and partnerships to address these issues. “The hope is that real, tangible actions will result,” said LIVESTRONG’s President and CEO, Doug Ulman.
Engaging and Empowering Patients
Patient engagement, empowerment, and navigation were strong themes throughout the meeting.
“We need communication about personalized medicine, … we need to pay attention to the psychosocial issues with targeted therapy, we need to put the person back in personalized medicine,” said Jimmie C. Holland, MD, who is Chair in Psychiatric Oncology at Memorial Sloan Kettering Cancer Center.
In one talk, Frederica Williams, MBA, FCIS (UK), President and CEO of Whittier Street Health in the Roxbury section of Boston, described a patient navigation program for the clinic’s mostly low-income, high-risk cancer patients. Although Dana-Farber Cancer Center is nearby, some of the Whittier Street patients were not comfortable going there, she said. After several years of planning, Whittier now has a community-based cancer center run by Dana-Farber in their building, staffed by medical oncologists and a nurse care coordinator. The nurse also serves as the patient navigator meets them at the door of the cancer center and guides them through their visit.
Not only are the Whittier Street patients getting excellent cancer care, she said, but clinical trial participation has increased dramatically. About 8.9% of the Whittier Street patients are participating in clinical trials—nearly three times the national average of 2.9%.
Patient navigation and engagement intertwines with the other key issues in personalized medicine. As Steven’s story showed, it is even important when it comes to tumor tissue testing, said Kimberly Allison, MD, a breast cancer pathologist at Stanford. Pathologists look for certain biomarkers routinely, such as estrogen receptor and HER2 status in breast cancer, she said, but it is not necessarily standard practice to test for the newer and less common markers, such as ALK in lung cancer.
“Patients need to know when to ask for additional testing,” she said. “Improving the quality of patient questions improves quality of care.” And the need for such questions is only going to grow.
Data Access
“The discovery of new mutation subtypes that might be targeted is going on rapidly now—every week or so there’s a new one,” said ASCO Immediate Past President Clifford A. Hudis, MD, FACP. “How can we make sure everyone has access to this information—that is our task.”
Making better use of electronic health records is one of the answers, he said. ASCO’s CancerLinQ, now in development, will enable physicians to enter their own patients’ records (de-identified) into a shared database. That will create a trove of data for analysis, feedback, and insight, helping to “ensure that every cancer patient and physician, wherever they are, has the very latest knowledge at their fingertips,” in the words of CancerLinQ’s website (www.asco.org/quality-guidelines/cancerlinq).
A related theme in the era of personalized medicine is the prominence of technology, not only for accessing data but also for patient empowerment.
“Technology gives us the ability to be our own advocate in conjunction with community,” said Alicia C. Staley, the CEO of Akari Health, a consulting group based in Boston. The company advises clients on how to use social media and social networks to build relationships with patient communities.
“Information is key to personalized medicine,” said another speaker, Gena Cook, CEO of Navigating Cancer in Seattle. Her company provides cancer programs with a branded, online patient education and support services.
Tangible Actions
After a day of presentations and roundtable discussions, participants split up into small groups to talk about possible solutions in the areas of patient engagement, quality of care including tissue diagnostics, and data access and technology.
In one of the tissue diagnostic groups, facilitator E. Blair Holladay, PhD, Executive Vice President of the American Society for Clinical Pathology, and others identified barriers to extensive biomarker testing, including the trend to smaller biopsies, which may not yield enough tissue for multiple tests and the need to bank tissue within an hour so the RNA remains intact.
They also discussed the need for more standardization and guidelines on what tests to perform for specific tumors. “The more [guidelines] the better,” said William Cance, MD, FACS, Surgeon-in-Chief at Roswell Park Cancer Institute.
Another group, with Stanford’s Dr. Allison, talked about the need for patient engagement at the tissue diagnostics stage. Ideas included making sure patients know that the treatment plan is based on tissue diagnostics, having an online portal with patient translations of pathologist report terms, and letting patients know they can get a second opinion on their tissue.
Ideas for action that emerged from all the groups will be included in a white paper on the forum. “Today was just the start,” said LIVESTRONG’s Mr. Ulman. “The actions to follow are key…. Interaction to action is our main objective.” ■
Disclosure: Drs. Holland, Williams, Allison, and Hudis, and Mr. Holladay reported no potential conflicts of interest.