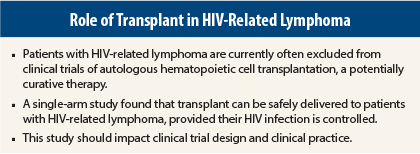
Human immunodeficiency virus (HIV)-positive patients with relapsed/refractory lymphoma can safely undergo autologous hematopoietic cell transplantation, according to results of a phase II multicenter trial presented at the 56th American Society of Hematology (ASH) Annual Meeting and Exposition in San Francisco.1 At many centers, HIV-positive patients with lymphoma are currently excluded from this potentially curative treatment due to concerns about increased risk of infection in these immunocompromised patients.
In the phase II trial, autologous hematopoietic cell transplantation achieved an estimated 1-year overall survival of 86.6% and progression-free survival of 82.3% in patients with HIV-related lymphoma who failed to respond to prior therapy. The estimated rate of disease progression at 1 year was 12.5%, and the estimated mortality was 5%.
Exclusion Unjustified
“Chemotherapy-sensitive patients with relapsed/refractory HIV-related lymphoma may successfully undergo [autologous hematopoietic cell transplantation] with favorable outcomes. Our study shows that exclusion from clinical trials on the basis of HIV infection alone is no longer justified. In fact, in clinical practice, patients with controlled HIV infection—with emphasis on the word “controlled”—should be receiving transplants as standard of care,” said lead study author Joseph Alvarnas, MD, Associate Clinical Professor and Director of Medical Quality at City of Hope, Duarte, California.
“Now that we have effective therapies for AIDS, we tend to trivialize it as a risk factor for lymphoma, but it is still a considerable risk factor. We have excellent treatment for patients with lymphoma, yet HIV infection remains an exclusion criterion for most [transplant] therapeutic trials. We conducted this study to see whether we could extend [autologous hematopoietic cell transplantation] to HIV-infected patients with lymphoma at nonspecialty centers,” he told an audience at a press conference held during the ASH meeting.
The single-arm, multi-institutional trial was conducted jointly by the Blood and Bone Marrow Transplant Clinical Trials Network and the AIDS Malignancy Clinical Trials Consortium. The 16 transplant centers included in the study do not necessarily specialize in HIV/AIDS treatment, therefore making it possible to duplicate the treatment at a broader number of nonspecialized centers, noted the authors.
Study Details
Study results were based on 40 HIV-infected patients with relapsed or refractory lymphoma. All underwent autologous hematopoietic cell transplantation, receiving a modified BEAM regimen (carmustine [BiCNU], etoposide, cytarabine, melphalan), and blood stem cell grafts. Antiretroviral therapy for HIV infection was withheld during the preparative regimen and resumed after the resolution of gastrointestinal toxicities. All patients received standard institutional supportive care posttransplant.
“Patients had no problem mobilizing stem cells,” Dr. Alvarnas said.
Dr. Alvarnas said that a historical case-control study of 151 matched non–HIV-infected patients with lymphoma who underwent autologous hematopoietic cell transplantation showed no significant differences in overall mortality compared with the HIV-infected patients in his team’s study. ■
Disclosure: The National Cancer Institute provided funding for the trial as part of the Cancer Therapy Evaluation Program to expand access to clinical trials for HIV-infected people with cancer. Dr. Alvarnas reported no potential conflicts of interest.
Reference
1. Alvarnas J, Le Rademacher, Wang Y, et al: Autologous hematopoietic stem cell transplant (AHCT) in patients with chemotherapy-sensitive relapsed/refractory human immunodeficiency virus (HIV)-associated lymphoma. 2014 ASH Annual Meeting. Abstract 674. Presented December 8, 2014.