The number of cancer survivors has been steadily increasing in recent years. According to the Ministry of Health National Cancer Registry, in 2010 there were 254,000 cancer survivors in Israel (3.3% of the population) compared with 15,700 (0.4% of the population, P < .005) in 1975.1 Forty years ago in the United States, cancer survivors made up about 1.5% of the general population (~3 million), whereas currently, about 4% of the U.S. population consists of cancer survivors (~14 million).2
On an international scale, according to the International Agency for Research on Cancer (IARC),3 there are over 30 million cancer survivors worldwide, and that number is expected to reach 70 million by 2050.4
Objectives
In 2009–2010, we conducted a study at Rambam Medical Center in Haifa, Israel, in which patients with breast and colorectal cancer were asked about needs that emerged during treatment and to what degree they were met. The patients had received adjuvant treatment with radiotherapy or chemotherapy and/or hormonal therapy, and at the time of the study, showed no signs of disease.
The patients were interviewed by a nurse, and upon completion of treatment, about 80% reported that most of their medical needs (ie, directly related to medical treatment for cancer) were met. In contrast, 67% of their needs related to physical functioning (as affected by the disease), 54% of their emotional needs, and only 44% of their practical needs (eg, related to work or financial situation) were met.5
Research Methods
In 2012, we resolved to conduct an additional similar survey, to refer survivors to entities that could help them with the needs they revealed, and to redo the survey 6 months after the referral. Thus, upon the completion of treatment, patients were interviewed by an oncology nurse regarding the frequency of their symptoms, and the nurse referred them to an attending entity accordingly.
Overall, 198 survivors diagnosed with breast and colorectal cancer participated in the new survey, upon the completion of radiotherapy, radiotherapy combined with chemotherapy, and radiotherapy combined with hormone therapy. All participants showed no signs of the disease. An authorization of the Helsinki Committee of the Rambam Medical Center was completed and obtained as required.
Among the 198 patients, 188 were females and 10 were males. The age range was 28.8 to 85.77 (mean, 58.2 ± 12.673). Of the women, 178 were diagnosed with breast cancer, and 10 with colorectal cancer. Almost all (99%) of the patients had undergone radiotherapy, 54% had received chemotherapy, and 64% had been given hormone therapy.
Questionnaire and Variables
The questionnaire encompassed nine symptoms that are frequently seen among survivors,6-9 according to our survey of the scientific literature (fatigue, pain, sleep disorders, cognitive dysfunction, emotional distress/depression, future anxiety, familial changes, financial distress/difficulties, weight changes). Patients were asked three questions about each symptom by the interviewing nurse, totaling 27 questions per each survivor. The answers were ranked from 1 to 5 according to the Likert scale (1 = never, 2 = rarely, 3 = sometimes, 4 = frequently, and 5 = always).
Reverse questions were arranged and scored accordingly (for example, to address familial changes, patients were asked to express their level of agreement with the statement, “I feel comfortable among household members”; to assess weight changes, they were asked to rank the statement, “I am at peace with my current look”).
Symptoms for which the resulting frequency ranking exceeded 2—occurring sometimes, frequently, or always—were considered disruptive.
Results
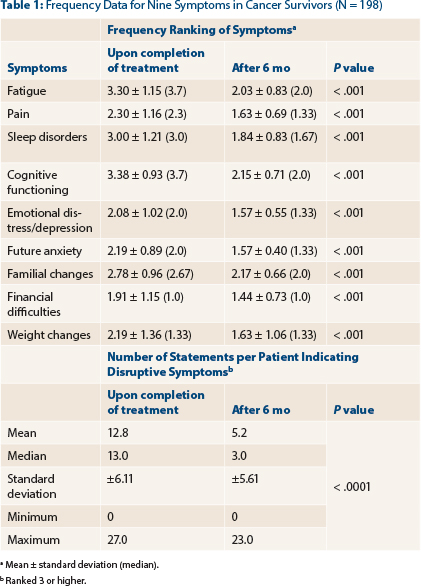
Table 1 shows the frequency ranking of the nine symptoms upon completion of treatment and after 6 months, and the statistical differences for each one of the symptoms. With the exception of financial distress, all the remaining symptoms were ranked higher than 2, indicating symptoms that are sometimes or frequently disruptive. No symptom was reported as being disruptive all the time.
The average number of statements indicating disruptive symptoms for patients upon completion of treatment was 12.8 ± 6.11 (median, 13). After 6 months, there was a significant drop in the number of responses suggesting disruptive symptoms (mean, 5.2 ± 5.6; median, 3; P < .001).
Education and Referrals
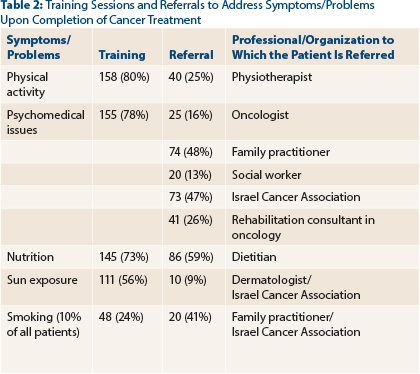
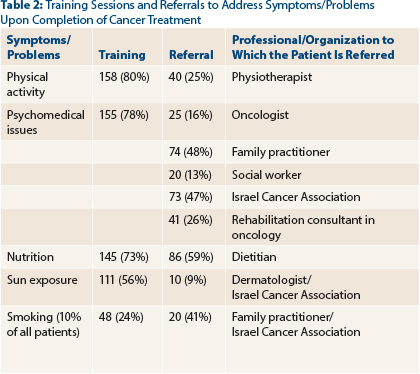
Training on nutrition, physical activity, and emotional support were delivered to between 73% and 80% of the survivors (Table 2). About half the survivors were referred to a family practitioner, a dietitian, and support activity provided by the Israel Cancer Association.
We see that most of the patients contacted a consultant who gave them advice upon completion of treatment: 96% contacted a family practitioner after having been referred, 94% contacted the Israel Cancer Association after having been referred to the organization upon completion of treatment, 93% contacted a dietitian after being referred upon completion of treatment (Table 3).
Discussion
In 1985, Fitzhugh Mullan, MD, a U.S. physician who had recovered from cancer, described the way he felt, in The New England Journal of Medicine, with these words: “It is as if we have invented sophisticated techniques to save people from drowning, but once they have been pulled from the water, we leave them on the dock to cough and splutter on their own in the belief that we have done all that we can.”10
As a result of this experience, Dr. Mullan became the founding President of the National Coalition for Cancer Survivorship in the United States, aimed at supporting cancer survivors. The Coalition acts on behalf of cancer survivors and endeavors to promote their well-being. The percentage of patients with a 5-year survival during the early years of the Coalition was around 55%, and today it has reached 69%.11,12
Dr. Mullan’s article apparently did not make great waves. But about 20 years later, in 2005, the U.S. Institute of Medicine—which, albeit an independent research institute, is counted among the health policymakers in the United States—published a paper entitled From Cancer Patient to Cancer Survivor: Lost in Transition.
The authors recommended efforts to increase awareness of the difficulties experienced by survivors, in terms of medical, functioning, and psychosocial problems derived from cancer and its treatment. They further recommended enhancing survivors’ quality of life by developing psychosocial support services.13,14
Within the context of the current study, we observed that patients with breast and colorectal cancer who showed no signs of these diseases upon completion of treatment suffered from other disorders. In most cases, the patient does not tell the physician about these symptoms and problems because, the way the patient sees it, the physician is busy with the medical problem and shouldn’t be bothered; this finding was also validated by research conducted in the United States.
For this reason, we asked the nurse to interview the patients and refer to the 27 statements pertaining to quality of life. Responses suggesting a disorder were reported for 12 of those statements. Following the initial survey, the nurse provided the survivors with support and/or referred them to entities that could provide them with assistance. This same nurse interviewed the patients 6 months later.
After 6 months, it emerged that the mean number of problematic statements dropped to 5. This is not a controlled study, and it is possible that some of the disorders would have resolved without any assistance. In our opinion, however, there is no doubt that patients have problems that should be clarified, and they should be provided with assistance, as required, while they are on the road to recovery.
Conclusions
It is important to monitor survivors,14-16 and there are numerous objectives to keep in mind: (1) detection of disease recurrence at an early stage, (2) treatment of side effects that can appear early or later as a result of treatment and/or the disease per se, (3) early detection of a secondary tumor that may emerge, and (4) assisting patients in coping with psychosocial challenges.
There are many ways to monitor survivors—by the oncologist in the oncology ward or by the family practitioner, in survivorship clinics or in clinics by disease type and location (eg, in breast or hematologic diseases). No prospective research has established which method is most effective, and there is always the need to review patients’ and caregivers’ wishes, as well as costs of each and every method. However, some studies have shown that survivors prefer to continue receiving support at the oncology support center where they were treated, while updating their family practitioner.17,20
Collaborative monitoring by the family practitioner and the attending oncologist, with the oncology nurse intermediating, appears to be the most cost-effective and efficient method. Therefore, it is essential that the family physician receive a detailed summary from the attending oncologist, describing the treatment summary of the survivor, including, inter alia, indication of late side effects that may derive from treatment. Forms for conveying this type of information were prepared by Ido Wolf, MD, with assistance from the Israel Cancer Association, and were coordinated with representatives of the Israeli Society for Clinical Oncology. ■
Disclosure: This study was partially financed by the Israel Cancer Association. The authors reported no potential conflicts of interest.
References
1. Keinan-Boker L: Deputy Director of the National Center for Disease Control of the Israel Ministry of Health [personal communication]. October 6, 2013.
2. Howlader N, Noone AM, Krapcho M, et al: SEER Cancer Statistics Review, 1975-2009. Bethesda, Maryland, National Cancer Institute, 2012.
3. Ferlay J, Shin HR, Bray F, et al: GLOBOCAN 2008 v1.2, Cancer incidence and mortality worldwide: IARC CancerBase No. 10. Lyon, France, International Agency for Research on Cancer, 2010. Available at http://globocan.iarc.fr.
4. World Cancer Research Fund/American Institute for Cancer Research. Cancer survivors, in Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective, pp 342-347. Washington, DC, AICR, 2007. Available at http://www.dietandcancerreport.org/cancer_resource_center/downloads/Second_Expert_Report_full.pdf.
5. Robinson E: Cancer survivors: A challenge to healthcare systems worldwide. International symposium. Panel discussion presented at 46th ASCO Annual Meeting, June 4-8, 2010.
6. Hsu T, Ennis M, Hood N, et al: Quality of life in long term breast cancer survivors. J Clin Oncol 31:3540-3548, 2013.
7. Helwick C: NCCN Clinical Practice Guidelines in Oncology: 2013 Updates. ASCO Post 4(8):3-10, 2013.
8. Mustian KM, Sprod LK, Janelsins M, et al: Multicenter randomized controlled trial of yoga for sleep quality among cancer survivors. J Clin Oncol 31:3233-3241, 2013.
9. Hollingworth W, Metcalfe C, Mancero S, et al: Are needs assessments cost effective in reducing distress among patients with cancer? A randomized controlled trial using the distress thermometer and problem list. J Clin Oncol 31:3631-3638, 2013.
10. Mullan F: Seasons of survival: Reflections of a physician with cancer. N Engl J Med 313:270-273, 1985.
11. American Cancer Society: Cancer Facts & Figures, 2013. Atlanta, American Cancer Society, 2013.
12. Hausman JH, Ganz PA, Sellers TP, et al: Journey forward: The new face of cancer survivorship. J Oncol Pract 7(3 suppl):e50s-e56s, 2011.
13. Hewitt M, Greenfield S, Stoval E: From cancer patient to cancer survivor: Lost in transition. Washington, DC, National Academies Press, 2006.
14. Jean-Pierre P, Winters PC, Ahles TA, et al: Prevalence of self-reported memory problems in adult cancer survivors: A national cross-sectional study. J Oncol Pract 8:30-34, 2012.
15. Furman MJ, Lambert LA, Sullivan ME, et al: Rational follow-up after curative cancer resection. J Clin Oncol 31:1130-1133, 2013.
16. Rosales AR, Byrne D, Burnham C, et al: Comprehensive survivorship care with cost and revenue analysis. J Oncol Pract 7:945-949, 2013.
17. Rechis R, Beckjord EB, Nutt S: Potential benefits of treatment summaries for survivors’ health and information needs: Results from a LIVESTRONG survey. J Oncol Pract 7:973-976, 2013.
18. Shalom MM, Hahn EE, Cassillas J, et al: Do survivorship care plans make a difference? A primary care provider perspective. J Oncol Pract 7:314-318, 2011.
19. Virgo KS, Lerro CC, Klabande CN: Barriers to breast and colorectal cancer survivorship care: Perceptions of primary care physicians and medical oncologists in the United States. J Clin Oncol 31:2322-2366, 2013.
20. Roordo C, Berendsen JA, Howenkamp, et al: Discharge of breast cancer patient to primary care at the end of hospital follow-up: A cross-sectional survey. Eur J Cancer 49:1836-1844, 2013.
Dr. Robinson is Professor of Oncology at Rambam Medical Center, Haifa, Chairman of the National Council for Oncology, and Chairman of the Israel Cancer Association, Givatayim. Ms. Gafni is a nurse in the Radiation Oncology Department at Rambam Medical Center. Ms. Muller is Director of Nursing in the Oncology/Hematology Division and Specialist in Palliative Care at Rambam Medical Center. Ms. Leiba is a statistician in the Quality Improvement Unit at Rambam Medical Center.