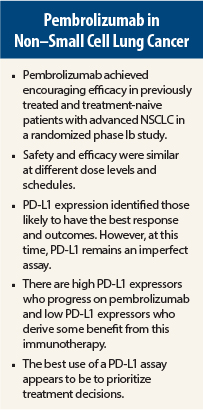
Add lung cancer to the growing list of cancers that may derive benefit from immunotherapy. The KEYNOTE-001 trial found that pembrolizumab (Keytruda) achieved durable responses in a proportion of patients with non–small cell lung cancer (NSCLC) and high levels of expression of the protein PD-L1 (programmed death ligand 1) in tumor tissue correlated with overall response rate and progression-free survival. These results suggest that PD-L1 is a potential, albeit imperfect, biomarker for response to anti–PD-1 therapy with pembrolizumab.
“With these data, we can confidently say that in previously treated patients with NSCLC and PD-L1 expression in at least 50% of tumor cells, pembrolizumab is associated with superior outcomes compared to what can be expected with cytotoxic chemotherapy,” stated Edward B. Garon, MD, of David Geffen School of Medicine at the University of California, Los Angeles.
No significant differences were observed in efficacy and side-effect profile between patients receiving various dose levels of pembrolizumab, which has been shown by other investigators, Dr. Garon noted.
Dr. Garon reported the KEYNOTE-001 results at the 2015 Annual Meeting of the American Association for Cancer Research,1 and the study was published in The New England Journal of Medicine to coincide with his presentation.2
Study Details
KEYNOTE-001 was a phase Ib study that assigned 495 treatment-naive and previously treated NSCLC patients receiving pembrolizumab at a dose of either 2 mg every 3 weeks or 10 mg/kg every 2 weeks to either a training group (n = 182) or a validation group (n = 313). PD-L1 expression was assessed in tumor samples.
Among all patients, the overall response rate was 19.4%, with no clear difference based on prior treatment, dose of pembrolizumab, or histology. As has been reported previously with immunotherapy, smokers had an improved response compared with never smokers. Median duration of response among responders was 12.5 months. Median duration of progression-free survival among all patients was 3.7 months, and median duration of overall survival was 12 months.
Pembrolizumab was generally well tolerated. The most common treatment-related adverse events were fatigue, pruritus, and decreased appetite, and these effects were similar at all dose levels.
PD-L1 Expression
In the training set, a cutoff point of at least 50% of cells that stained positive for PD-L1 was deemed highly positive. In the validation set, three proportion scores were used to categorize PD-L1 expression: proportion score < 1% = low; proportion score = 1% to 49% = intermediate; proportion score ≥ 50% = high. The validation set included 313 patients (223 previously treated, 90 treatment-naive to systemic therapy for NSCLC).
PD-L1 staining correlated with response, with no difference in previously treated or treatment-naive patients. In those with a proportion score ≥ 50% (the highest expression of PD-L1), the overall response rate was 42.5%; median progression-free survival was 6.3 months, and median overall survival had not yet been reached. The overall response rate was significantly better in high expressors than in those with a proportion score of between 1% and 49% and those with a proportion score < 1% (P < .001).
Progression-free survival in pooled data from the training and validation set showed a correlation with high PD-L1 expression. Median progression-free survival according to PD-L1 expression was 6.3 months for the highest group vs 3.3 months for the intermediate group and 2.3 months for the lowest PD-L1–expressing group.
At a median follow-up of 10.9 months, median overall survival was not reached in those with the highest proportion score (≥ 50%) in both previously treated and treatment-naive patients. In the previously treated patients, median overall survival was 7.3 months for those with a proportion score of 1% to 49% and 8.6 months for the lowest PD-L1–expressing group; in the treatment-naive patients, median overall survival was 16.2 months for the intermediate group and 10.4 months for the lowest PD-L1–expressing group.
“The PD-L1 level also [correlated with] overall survival,” Dr. Garon told The ASCO Post. “There is no real distinction in my mind between the quality of the data for progression-free and overall survival,” he said.
Dr. Garon pointed out that the efficacy of pembrolizumab in patients with low expression of PD-L1 was also “compelling.”
Blurry Biomarker
“These are very exciting results in advanced NSCLC,” stated Suzanne Topalian, MD, of Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore. “This is a difficult-to-treat patient population. Second- and third-line agents are not expected to prolong survival, so results are especially impressive in this setting.”
Dr. Topalian was less enthusiastic about the potential for PD-L1 as a biomarker for preselecting patients for therapy. “This is more clear-cut with tyrosine kinase inhibitors, where biology tells us that if a patient does not have a specific mutation, the therapy will not work. This biomarker is a lot more blurry than a BRAF mutation in melanoma, for example. Patients with lower PD-L1 staining still had a response.”
“In this study, highly PD-L1–positive patients were more likely to respond to pembrolizumab, but there is still a group of patients who are marker-negative who do respond. PD-L1 might be used to stratify patients who are more likely to respond and to prioritize the use of pembrolizumab. For example, if a patient with NSCLC has a proportion score ≥ 50%, pembrolizumab could be a good first choice, but another patient with low PD-L1 expression might be a better candidate for first-line chemotherapy,” she continued.
Combinations and sequencing of immunotherapies are the next important areas of study. PD-L1 expression could be used to prioritize combinations and sequencing, she added. ■
Disclosure: The study was funded by Merck. Dr. Garon’s institution received funds to conduct the trial.
References
1. Garon EB, Rizvi N, Hui R, et al: Efficacy of pembrolizumab (MK-3475) and relationship with PD-L1 expression in patients with non-small cell lung cancer. 2015 AACR Annual Meeting. Abstract CT104. Presented April 19, 2015.
2. Garon EB, Rizvi N, Hui R, et al: Pembrolizumab for the treatment of non-
small-cell lung cancer. N Engl J Med. April 19, 2015 (early release online).