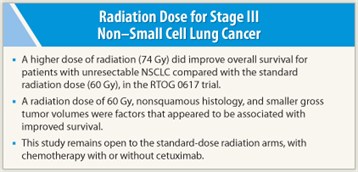
Surprisingly, less may be more when it comes to radiation therapy with concurrent chemotherapy for patients with stage III non–small cell lung cancer (NSCLC), according to an interim analysis of the randomized phase III Radiation Therapy Oncology Group (RTOG) 0617 trial presented at the 53rd Annual Meeting of the American Society for Radiation Oncology (ASTRO).1 A higher dose of radiation (74 Gy) does not appear to improve overall survival for patients with unresectable NSCLC compared with the standard radiation dose (60 Gy).
 “Although the optimal radiation dose for lung cancer patients has not been tested in a randomized phase III trial for over 30 years, most [radiation oncologists] believed that higher doses of radiation cured more patients with lung cancer,” revealed presenting author of this study, Jeffrey Bradley, MD, a radiation oncologist at the Washington University School of Medicine in St. Louis. Although Dr. Bradley admits that many centers have been using the higher dose of radiation for these patients, he and his colleagues believe that the standard radiation dose should remain 60 Gy, based on these preliminary findings.
“Although the optimal radiation dose for lung cancer patients has not been tested in a randomized phase III trial for over 30 years, most [radiation oncologists] believed that higher doses of radiation cured more patients with lung cancer,” revealed presenting author of this study, Jeffrey Bradley, MD, a radiation oncologist at the Washington University School of Medicine in St. Louis. Although Dr. Bradley admits that many centers have been using the higher dose of radiation for these patients, he and his colleagues believe that the standard radiation dose should remain 60 Gy, based on these preliminary findings.
Crossing the Futility Boundary
Between November 2007 and April 2011, 426 patients with newly diagnosed stage III NSCLC took part in RTOG 0617, perhaps the largest study to date to ask the question of radiation dose in stage III lung cancer. Patients were randomized to one of four treatment arms: high-dose (74 Gy) radiation therapy vs standard-dose (60 Gy) radiation therapy and concurrent chemotherapy with or without cetuximab (Erbitux). Concurrent chemotherapy included weekly paclitaxel and carboplatin. Two types of external-beam radiotherapy were used during the trial: three-dimensional conformal radiation therapy (3D-CRT) and intensity-modulated radiation therapy (IMRT). “This is the first phase III trial to allow IMRT in lung cancer,” declared Dr. Bradley.
 Preliminary study analysis showed that projected 12-month overall survival rates were higher with the standard 60-Gy radiation dose than with the higher 74-Gy dose (81% vs 74%), although Dr. Bradley acknowledged that the median follow-up was “rather short.” In addition, there did not appear to be a difference in outcomes based on which type of radiation therapy was used. (3D-CRT was used in 55% of patients, whereas IMRT was used in 45% of patients.) There appeared to be no statistical difference between the arms in terms of toxicity.
Preliminary study analysis showed that projected 12-month overall survival rates were higher with the standard 60-Gy radiation dose than with the higher 74-Gy dose (81% vs 74%), although Dr. Bradley acknowledged that the median follow-up was “rather short.” In addition, there did not appear to be a difference in outcomes based on which type of radiation therapy was used. (3D-CRT was used in 55% of patients, whereas IMRT was used in 45% of patients.) There appeared to be no statistical difference between the arms in terms of toxicity.
After 90 events (deaths) had occurred, it was determined that the high-dose radiation arms had crossed the “futility boundary.” The high-dose radiation arms were closed, and the study remains open to the standard-dose radiation arms, with chemotherapy with or without cetuximab. Planned completion of the trial is expected later in the fall of 2011.
Predictors of Survival
In an attempt to explain why the higher dose of radiation did not improve overall survival, the investigators are still carefully reviewing their data. Age, histology, gender, gross tumor volume, and total lung volume were considered as possible covariates predicting survival. However, according to Dr. Bradley, radiation technique and PET staging were not significant in predicting overall survival. The investigators concluded that radiation dose of 60 Gy, nonsquamous histology, and smaller gross tumor volumes were factors that appeared to be associated with improved survival. ■
Disclosure: Dr. Bradley reported no potential conflicts of interest.
Expert Point of View: No Improvement in Survival with High-dose over Standard-dose Radiation for Stage III Non–Small Cell Lung Cancer
Reference
1. Bradley JD, Paulus R, Komaki R, et al: Randomized phase III comparison of standard-dose (60 Gy) versus high-dose (74 Gy) conformal chemoradiotherapy ± cetuximab for stage IIIA/IIIB non-small cell lung cancer: Preliminary findings on radiation dose in RTOG 0617. 53rd ASTRO Annual Meeting. Abstract LBA2. Presented October 3, 2011.

