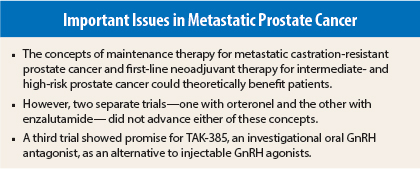
Despite the proliferation of new drugs to treat prostate cancer, further progress is proving somewhat elusive, according to three trials presented at the 2015 European Cancer Congress.
One study had positive results with orteronel maintenance therapy in patients with metastatic castration-resistant prostate cancer stabilized on docetaxel, but that drug has been abandoned.1
A second trial showed lackluster results for neoadjuvant therapy with enzalutamide (Xtandi) earlier in the course of disease.2
A third trial provided a glimmer of hope improving hormonal therapy with TAK-385, an oral antagonist under development.3
Orteronel: Not an Option
Orteronel, a drug that was developed to be a more selective nonsteroidal androgen synthesis inhibitor, was studied in a phase III trial as maintenance therapy. “Maintenance therapy has proven effective in other malignancies,” explained senior author Silke Gillessen, MD, of Kantonsspital St. Gallen, St Gallen, Winterthur, Switzerland, providing a rationale for the trial.
“In this trial, orteronel significantly improved event-free survival and radiographic progression-free survival as switch maintenance therapy. It was generally well tolerated in patients with disease stabilization after docetaxel. Although there was increased toxicity in the orteronel arm, it was manageable. To our knowledge, this is the first trial using a novel androgen receptor pathway inhibitor as switch maintenance therapy in prostate cancer.”
The study was initiated before development of orteronel was discontinued in June 2014, when it failed to prolong survival compared with prednisone alone in chemotherapy-naive metastatic castration-resistant prostate cancer.
At time of premature termination of the trial, 47 patients with metastatic castration-resistant prostate cancer who had not progressed after first-line docetaxel had been enrolled. Patients continued on androgen-deprivation therapy and were randomized 1:1 to receive orteronel plus best supportive care or placebo plus best supportive care.
The primary endpoint was event-free survival. Prostate-specific antigen (PSA) rise alone (biochemical failure) was not considered an event. The trial was stopped prematurely, with only 47 patients enrolled. Median follow-up is 17 months for patients on orteronel and 18.4 months for patients on placebo.
Median event-free survival was significantly better for orteronel: 8.5 months vs 2.9 months for placebo, which was shorter than anticipated (P = .001), Dr. Gillessen said.
Radiographic progression-free survival was 8.5 months with orteronel vs 2.8 months with placebo (P = .02).
In the orteronel group, 57% of patients had at least a 50% decline in PSA from baseline vs 4% of the placebo group. Time to PSA progression was 6.5 months vs 1.8 months (P = .004). “This study suggests that the concept of maintenance should be further investigated,” Dr. Gillessen told listeners.
“Although orteronel is no longer being developed, the results show that pathway receptor inhibitors could have therapeutic potential in this setting and, as such, deserve further investigation,” wrote John Yarnold, MD, in the daily newspaper at the 2015 European Cancer Congress. He is Professor at the Institute of Cancer Research and Royal Marsden Hospital, NHS Foundation Trust, London, and was not involved in this study.
Enzalutamide Evaluated as Neoadjuvant Therapy
Neoadjuvant therapy improves pathologic complete response rates and overall survival in other solid tumors, such as breast, lung, colorectal, and bladder cancers. A randomized phase II study evaluated the role of neoadjuvant therapy with enzalutamide given 6 months before radical prostatectomy in 52 patients with intermediate- and high-risk, node-negative, localized prostate cancer. Patients were randomized to receive triple therapy with enzalutamide/leuprolide/dutasteride or enzalutamide alone, in an attempt to destroy micrometastasis that may persist after surgery for prostate cancer.
“On the one hand, the glass is half full: We replicated results of the abiraterone study. On the other hand, the glass is half empty: We did not see pathologic complete responses in the 20%–25% range, which would justify going on to phase III trials in this population,” said lead author Bruce Montgomery, MD, of the University of Washington, Seattle.
Pathologic complete response was achieved in two patients (9%) in the triple-therapy arm and none in the monotherapy arm. At prostatectomy, 26% of the triple-therapy arm and 4% of the monotherapy arm were found to be node-positive.
Dr. Montgomery said that the rates of node positivity in these patients requires further molecular study, and he is in favor of continued efforts to identify optimal neoadjuvant combination therapy with higher pathologic complete response rates to justify randomized phase III trials.
“The short answer is that we did not ablate the androgen receptor signal,” Dr. Montgomery added. “We have hope that we have room to move to further suppress androgen receptor signaling with other combinations and novel agents,” he told listeners.
Proffered Paper Session Co-Chair, Richard Cathomas, MD, of Kantonsspital Graubünden, Switzerland, said, “With neoadjuvant enzalutamide monotherapy, we do not see many pathlogic complete responses despite high PSA responses. Outside of clinical trials, there is no role for neoadjuvant therapy. At this juncture, radiation and androgen-deprivation therapy are considered standard salvage therapy options.”
TAK-385, Oral GnRH Antagonist
First results of a randomized phase II trial in patients with biologically confirmed prostate cancer who were candidates for first-line androgen-deprivation therapy were encouraging for TAK-385 vs leuprolide.
TAK-385 is an oral gonadotropin-releasing hormone (GnRH) antagonist with the potential to improve cardiovascular safety and convenience compared with injectable GnRH androgen-deprivation therapy, which is widely used to treat locally advanced metastatic castration-resistant prostate cancer.
“TAK-385 is potentially the first-in-class oral medication to achieve rapid reduction of testosterone. PSA responses were rapid and occurred during the first 4 weeks. Compliance was high, and efficacy was achieved. The interim analysis of the phase II trial revealed no new safety signals. TAK-385 is more convenient than an injectable GnRH agonist,” said lead author Neal Shore, MD, of Carolina Urologic Research Center, Myrtle Beach, South Carolina.
Final results are awaited, and further phase II studies will guide future development, he said. “We did not get to a maximal tolerated dose in terms of toxicity, and the drug was well tolerated in young men and the elderly. We saw excellent testosterone suppression at 24 weeks. We await data in a radiation therapy cohort, and then we will decide on the dose for phase III,” he told listeners.
The study randomized patients who were candidates for first-line androgen-deprivation therapy to TAK-385 80 mg/d (n = 50), TAK-385 100 mg/d (n = 50), or leuprolide subcutaneously every 12 weeks (n = 25). No visceral or lung metastases were allowed.
The primary endpoint of the trial was testosterone suppression. TAK-385 achieved consistent testosterone suppression rapidly, with a reduction to castrate levels seen by day 7 that was sustained out to 6 months. No testosterone surge was observed with TAK-385, whereas a surge in testosterone was observed with leuprolide over the first week, followed by eventual testosterone suppression.
“This is the first demonstration in an oral formulation of a GnRH antagonist, and it is a nice demonstration of efficacy,” Dr. Shore told listeners.
Drug-related adverse events were similar in all three arms. No treatment discontinuations were needed due to hepatic toxicity. ■
Disclosure: Dr. Gillessen is on the advisory board of Curevac, Dendreon, Janssen Cilag, Janssen Diagnostics, Novartis, Orion Pharma, Pfizer, Millennium Pharmaceuticals, Astellas, Sanofi Aventis, and Bayer (compensated), ProteoMediX and ESSA Pharmaceuticals Corp. (uncompensated); is on the speakers bureau of Amgen, Bayer, Janssen Cilag, and Sanofi Aventis (without honorarium); and has a patent application for a method for biomarker WO 2009138392 A1. Dr. Montgomery disclosed financial relationships with Medivation, Janssen, Tokai, and ESSA Pharma. Dr. Shore has received financial support from Millennium Pharmaceuticals. Drs. Yarnold and Cathomas reported no potential conflicts of interest.
References
1. Cathomas R, Crabb S, Kenner H, et al: Orteronel maintenance therapy in patients with metastatic castration resistant prostate cancer and non-progressive disease after first-line docetaxel therapy: Results of a multicenter randomized double-blind placebo-controlled phase III trial (SAKK 08/11). 2015 European Cancer Congress. Abstract 2500. Presented September 26, 2015.
2. Montgomery B, Joshua A, Gleave M, et al: A randomized, open-label, phase 2 study of enzalutamide as neoadjuvant therapy for patients undergoing prostatectomy for localized prostate cancer. 2015 European Cancer Congress. Abstract 2501. Presented September 26, 2015.
3. Shore N, Bailen J, Pieczonka C, et al: TAK-385, an oral GnRH antagonist: Efficacy and safety results from a randomized phase 2 trial in prostate cancer patients. 2015 European Cancer Congress. Abstract 2502. Presented September 26, 2015.