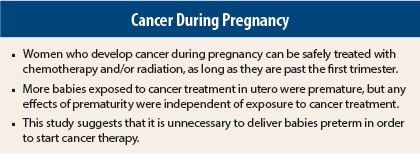
Children with in utero exposure to chemotherapy and/or radiation therapy during maternal treatment for cancer had no impairment in cognition, cardiac function, and general early childhood development, according to a study reported at the European Cancer Congress in Vienna, Austria, and published simultaneously online in The New England Journal of Medicine (see related article).1,2 Although prematurity generally was correlated with a worse cognitive outcome, this effect was independent of exposure to chemotherapy—which is a novel finding.
“Currently women who develop cancer and require treatment have preterm delivery so that treatment can start. These results show that preterm delivery—but not cancer treatment—is associated with worse outcomes,” said lead author Frederic Amant, MD, who is Assistant Professor, Staff Gynecologic Oncologist, and Head of the Scientific Section of Gynecologic Oncology at University Hospitals Leuven in Leuven, Belgium. “This suggests that we should no longer induce preterm delivery and that it is safe to start cancer treatment while a woman is pregnant, except during the first trimester,” he said.
“We hope that with these data, we can convince more oncologists around the world to treat cancer during pregnancy and avoid preterm delivery,” he told listeners at a press conference held during the Vienna meeting.
The moderator at the press conference, Elisabeth de Vries, MD, PhD, said, “I don’t have to be convinced. We are already convinced that it is good to share these data on how to behave and what to expect [in this setting].” Dr. de Vries is Head of the Department of Medical Oncology at the University Medical Centre Groningen, the Netherlands.
Study Design
The multicenter, case-control study enrolled 129 children whose mothers had cancer (prenatal exposure group) and matched them 1:1 to 129 controls from the general population who were born to healthy mothers after uncomplicated pregnancies and deliveries.
Dr. Amant said that 3 years ago, the first interim results were reported with no control group. The main novel finding of current results is that chemotherapy and radiation had no deleterious effects on preterm babies.
A total of 96 women in the exposure group were exposed to chemotherapy alone, 11 to radiation alone, and 13 to surgery alone; 4 of these women had both radiation and surgery, and 7 had chemotherapy and radiation. Fourteen women had no treatment because they were diagnosed late in their pregnancies, so they were treated post delivery.
Birth Data
Overall, 61% of births in the study were preterm, defined as before 37 weeks of gestation. This rate is much higher than in the general population (6.8%–8%), Dr. Amant noted. Eleven children were born between 27 and 32 weeks of gestation, 16 between 32 and 33.9 weeks, 52 between 34 and 36.9 weeks, and 50 at 37 weeks (full-term). The numbers and types of congenital malformations were similar between cases and controls.
The main assessments were the health of babies, cognitive outcome, and cardiac morphology and function. All children were tested at 18 months, and 48 children were tested at both 18 months and 36 months.
Birth weight was below the 10th percentile (defined as small for gestational age) in 28 children (22%) in the prenatal exposure group and in 19 control children (15.2%), a difference that was not statistically significant. Looking more closely, the rates of “small for gestational age” were 25% in children exposed to chemotherapy and 36% in children exposed to radiotherapy. Among children whose mothers received chemotherapy and were small for gestational age, 64% had catchup weight at the time of testing, Dr. Amant said.
Other Outcomes
For general health (incidence of medical problems, need for surgery and/or medical care), there was no difference between study children and controls.
Cognitive outcome was assessed at a median age of 22 months using the Bayley Scales of Infant Development. There were no significant differences in cognitive outcomes between the prenatal exposure group and controls.
“Cognitive results were the same in those exposed to chemotherapy, to radiation, and to surgery alone. This is reassuring,” Dr. Amant stated.
No difference in cognitive function was seen between children exposed to one or two cycles of chemotherapy and those exposed to six or seven cycles of chemotherapy, he added. Additionally, no differences in cognitive function were observed according to the type of chemotherapy.
Previous studies have shown a wide variation in cognitive outcome associated with prematurity, with generally worse outcomes in premature children, he told listeners.
Cardiac function was assessed at 36 months in 50 of 54 children using electrocardiography and echocardiography, and 47 children had sufficient data for evaluation. These children were compared with 47 matched controls for age and sex. No structural abnormalities were seen in any of the children, and no differences in any cardiac parameter assessed were observed between exposed children and controls.
Bottom Line
“What is new in this study is that the negative effect of prematurity is the same for [children exposed to cancer therapy] and controls,” he emphasized. “If we look at children antenatally, no one can see the difference in cognition and cardiac function between exposed children and other children.”
Most mothers had breast or blood cancers treated with anthracyclines. Dr. Amant said although heart function in the exposed babies was normal, long-term monitoring is advised for those whose mothers received anthracyclines.
Dr. Amant emphasized that these findings apply to treatments used in this study and cannot be extrapolated to newer targeted agents. n
Disclosure: The study was funded by the Belgian Cancer Plan. For full disclosures of the study authors, visit www.nejm.org.
References
1. Amant F: Cancer in pregnancy. European Cancer Congress. Special Session. Presented September 28, 2015.
2. Amant F, et al: Pediatric outcome after maternal cancer diagnosed during pregnancy. N Engl J Med. September 28, 2015 (early release online).