A new guidance statement from ASCO and the American Academy of Hospice and Palliative Medicine (AAHPM) could potentially lead to more standardized primary palliative care delivery across oncology settings, according to Kathleen E. Bickel, MD, MPhil, who presented the study findings at the 2015 Palliative Care in Oncology Symposium in Boston.1
When integrated into routine oncology care, palliative care improves symptom burden, quality of life, and patient and caregiver satisfaction. However, not all patients with cancer have access to specialist palliative medicine.
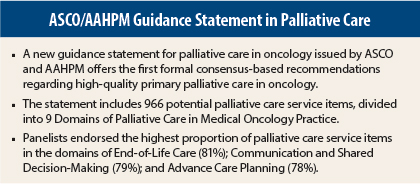
“This work is a joint guidance statement to define high-quality primary palliative care delivery in medical oncology,” said Dr. Bickel, Assistant Professor of Medicine, White River Junction Veterans Affairs Medical Center and Geisel School of Medicine at Dartmouth, Hanover, New Hampshire. This statement provides the first formal consensus-based recommendations regarding high-quality primary palliative care in oncology.
‘Real Tools’
“Serious illness is hard, and there’s a lot we want our medical team to do for us,” Dr. Bickel said. “This guidance statement is intended to represent what oncology clinic stakeholders feel right now is reasonable, important, and feasible to implement in current practice.”
Consistent access to at least basic palliative care services would be improved if the delivery of high-quality primary palliative care services were incorporated into all medical oncology practices. “The purpose of this project is to give oncology practice real tools to improve their delivery of primary palliative care,” she said.
Investigators sought to determine which palliative care elements constitute high-quality palliative care delivery in U.S. medical oncology practices, for adult patients with advanced cancer or a high symptom burden.
Domains of Palliative Care
An expert steering group of committee members from AAHPM and ASCO developed a list of 966 potential palliative care service items, divided into 9 Domains of Palliative Care in Medical Oncology Practice, each describing an aspect of palliative care delivery for patients with advanced cancer.
The domains were defined as follows: Symptom Assessment and Management, Psychosocial Assessment and Management, Spiritual and Cultural Assessment and Management, Communication and Shared Decision-Making, Advance Care Planning (including ethical and legal issues), Coordination and Continuity of Care, Appropriate Palliative Care and Hospice Referral, Caregiver Support (family/caregiver and staff), and End-of-Life Care. Service items were also categorized by composite ratings of “include,” “uncertain,” or “exclude.”
Ranking Each Service
Panelists included 22 physicians and 9 others (nurses, social workers, or patient advocates). “We wanted to ask what piece of the palliative care pie do the oncology stakeholders feel like they can own,” Dr. Bickel explained.
“Palliative care is a huge domain. We wanted to find out what oncology practices should be trying to focus on vs what they feel they should have other people help them with—what happens in the oncology practice rather than what is delivered by a palliative care specialist.”
The 31 multidisciplinary panelists ranked each service item according to importance (within the medical oncology office, how essential is this item/service to the delivery of high-quality care to patients with advanced cancer), feasibility (how feasible is it for a practice like yours, or the practices you interact with most, to provide this item/service), and scope of practice (how reasonable is it to expect that this item/service should be provided by medical oncology practices).
“We did not ask panelists to consider strength of evidence or recommendations from other organizations when ranking,” said Dr. Bickel. “We wanted panelists’ general feelings about ‘real-world’ practice.”
Highest Consensus in End-of-Life Care
Panelists endorsed the highest proportion of palliative care service items in the domains of End-of-Life Care (81%); Communication and Shared Decision-Making (79%); and Advance Care Planning (78%). The lowest proportions were in Spiritual and Cultural Assessment and Management (35%) and Psychosocial Assessment and Management (39%).
“In the largest domain, Symptom Assessment and Management, there was consensus that all symptoms should be assessed and managed at a basic level, with more comprehensive management for common symptoms such as nausea, vomiting, diarrhea, dyspnea, and pain,” said Dr. Bickel.
Of the 966 potential palliative care service items, the consensus panel rated 598 items (62%) as “include” (important, feasible, and within the scope of oncology practice) and 21 (2%) as “exclude,” whereas 347 (36%) were rated as “uncertain.”
Guidance Not Guidelines
Oncology providers wishing to enhance palliative care delivery may find the guidance useful to inform operational changes and quality improvement efforts, but “this is a guidance statement; these are not guidelines,” Dr. Bickel stressed. However, metric development may be informed by the data from this consensus process.
“I think it’s critically important for there to be guidance to set forth what are the domains of primary palliative care for cancer, and this is a first step in an effort that seems quite successful,” said Kathleen M. Foley, MD, Attending Neurologist Pain & Palliative Care Service, Memorial Sloan Kettering Cancer Center (MSKCC) and Chair, Society of MSKCC in Pain Research, New York.
“I see it as a first step that gives the opportunity, for everyone now, to respond to it, to see how they can implement it, and more importantly, refine it,” Dr. Foley told The ASCO Post.
“We’re not saying that everyone must do these things starting tomorrow,” added Dr. Bickel. “But this is what a group of real people in the trenches thought to be a reasonable starting place for oncologists to try to start doing palliative care themselves.”
She continued: “These goals may adapt and change over time, but we hope this work will serve as a foundation for future palliative care–related quality measures, quality improvement initiatives, and educational activities.” ■
Disclosure: Dr. Bickel reported no potential conflicts of interest.
Reference
1. Bickel KE, McNiff KK, Buss MK, et al: Defining high-quality palliative care in oncology practice: An ASCO/AAHPM Guidance Statement. 2015 Palliative Care in Oncology Symposium. Abstract 108. Presented October 10, 2015.