Surgeons at the cutting edge are offering minimally invasive resection to patients with small gastrointestinal stromal tumors (GISTs) deemed to be low-risk, according to panelists at a session of the American College of Surgeons 2014 Clinical Congress in San Francisco.
“We are seeing more small GISTs due to increased screening, and they will be amenable to hybrid resection [endoscopy/laparoscopy] or pure endoscopic resection,” said Lee L. Swanstrom, MD, FACS, Clinical Professor of Surgery at Oregon Health Sciences University and Director of GI and Minimally Invasive Surgery for Legacy Health System in Portland. Dr. Swanstrom is also Chief Innovations Officer at the IHU Strasbourg in Strasbourg, France.
“Endoscopic resection is demanding, but it has been shown to be safe and feasible for the right indications. Improvements in flexible endoscopic tools will make such resections quicker and easier in the near future,” Dr. Swanstrom said.
Not All GISTs Require Resection
Chandrajit P. Raut, MD, MSc, Associate Professor of Surgery at Harvard Medical School and Surgery Director of Sarcoma at Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston, noted that GISTs are “exceedingly common, but most are clinically irrelevant.” He said that about 5,000 GIST cases are diagnosed in the United States each year, but submucosal microscopic lesions (ie, those < 1 cm) occur more frequently.
Submucosal microscopic GISTs have been identified in 35% of stomachs removed for gastric cancer and in more than 20% of autopsy specimens. “Certainly, they don’t all require surgery,” Dr. Raut noted.
Among GISTs < 2 cm, resection is recommended for lesions that are symptomatic, ulcerated, and enlarging. For those < 2 cm without high-risk features—irregular borders, cystic spaces, ulceration, echogenic foci, and heterogeneity—endoscopic surveillance at 6- to 12-month intervals can be considered, according to the guidelines of the National Comprehensive Cancer Network (NCCN). Surgery is indicated when GISTs increase in size or become symptomatic, he said.
Field F. Willingham, MD, MPH, Director of Endoscopy and Assistant Professor of Medicine at Emory University School of Medicine, Atlanta, agreed that the patient with a submucosal mass < 2 cm and no suspicious features on endoscopic ultrasound can be considered for surveillance.
“The NCCN has adopted this, and we think it’s a reasonable way to go for these small lesions,” he said.
“We need to figure out who will progress,” Dr. Raut added. Radiology, endoscopy, histopathology, and molecular diagnostics all have shortcomings in determining which small lesions are aggressive, he added.
“Endoscopic biopsy using standard biopsy forceps is not usually helpful for submucosal tumors. Mitotic count can help identify which to resect but cannot be accurately assessed on endoscopic ultrasound–guided fine-needle aspiration specimens. Tumors < 2 cm vs those > 2 cm have an excess of wild-type cases, compared with known mutations, so they appear to be a different subpopulation with less proliferation potential,” Dr. Raut suggested.
Minimally Invasive Resections
For small tumors that warrant resection, laparoscopic and endoscopic approaches are emerging, although they are still highly experimental in North America. Dr. Willingham described a “hybrid” technique that partners endoscopic with laparoscopic techniques and that succeeds in obtaining negative margins in GISTs not amenable to standard laparoscopic wedge resection. He and his colleagues at Emory developed this approach as part of their aim to offer a less invasive treatment to GIST patients.
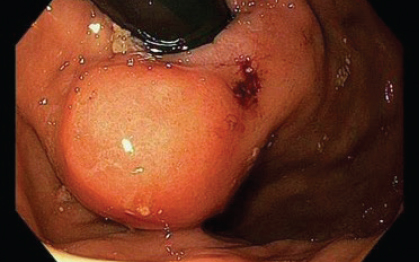
Dr. Willingham noted that standard GIST surgery can involve a major gastric resection, especially for lesions at the gastroesophageal junction and in the proximal cardia, which are difficult locations for wedge resection (Fig. 1). “This led us to think of ways we could work together [with surgeons] to offer less invasive therapy in this area, especially for small, nonaggressive tumors,” he said.
Their technique, which they call a “push-pull endoscopic and laparoscopic full-thickness resection,” addresses the deep margins of the tumor in a minimally invasive way. In a study of four patients with challenging disease, they found that endoscopic resection alone was associated with a positive deep margin, but a negative margin was achieved after a laparoscopic, full-thickness resection that accompanied the endoscopy.1
“The advantages of this technique are that it is minimally invasive, does not require major organ resection, and provides a full-thickness resection of the involved deep margin,” he explained.
Endoscopic submucosal dissection is another emerging minimally invasive approach to GIST. This procedure is still emerging in the United States but is in widespread use in Asia, where more than 50% of foregut digestive cancers are treated via flexible endoscopy rather than surgical resection, Dr. Swanstrom reported. He predicted that the trend will grow in the Western world as well.
He cautioned that endoscopic resection of GISTs is only indicated for lesions that are small (< 5 cm), located in the esophagus or stomach, and demonstrate low-risk characteristics.
“As our instrumentation in flexible endoscopy becomes more sophisticated, with better ways to control energy and with oncologic tools such as specimen retrieval sacs, we will see an expansion of endoscopic submucosal dissection,” Dr. Swanstrom predicted. “We no longer fear doing full-thickness resections in the gut, as we once did.”
Dr. Raut added a note of caution. “Ultimately, GIST is a cancer, and oncologic principles trump whatever observational or operative approach we use. We need to do what’s most appropriate oncologically.” Dr. Raut does not advocate for a pure endoscopic excision, and this is not routinely performed at his institution. Instead, he favors a laparoscopic or combined laparoendoscopic approach, which allows removal of the tumor with a margin of normal tissue.
David A. Kooby, MD, Professor of Surgery, Emory University School of Medicine, Atlanta, called the minimally invasive approaches to GIST, “innovative, wonderful stuff.”
“Where we are now and where we will be in 5 to 10 years are very different. The use of endoscopy for lower-risk tumors would be a great advantage over our standard approach, which is to remove a big portion of the stomach,” Dr. Kooby noted. “If we can do this minimally invasively, as these speakers have described, and adhere to oncologic principles, this will optimize treatment.” ■
Disclosure: Dr. Swanstrom has received research and education support and/or consulted for Boston Scientific, Olympus, Aponos, Covidien, Cardica, Endogastric Solutions, Titan, Stryker, Fractyl, and Apollo. Drs. Willingham, Raut, and Kooby reported no potential conflicts of interest.
Reference
1. Reynolds PT, et al: Hybrid push-pull endoscopic and laparoscopic full-thickness resection for the minimally invasive management of gastric gastrointestinal stromal tumors. Gastroenterology 146(5 suppl 1):S-1051–S-1052, Abstract Su1847, 2014.