A small phase I/II clinical study from Johns Hopkins University in Baltimore found that epigenetic therapy with a combination of azacitidine (Vidaza) and entinostat (an investigational agent) produced responses in some patients with refractory advanced non–small cell lung cancer. The study results, published in a recent issue of Cancer Discovery,1 showed a median survival of 6.4 months in patients who had a median of three prior therapies for their lung cancer, more than 2 months longer than the usual 4-month survival rate in this population.
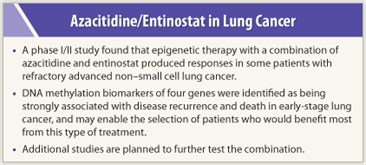 Of the 45 patients enrolled in the study, all of whom received the epigenetic treatment, 19 were able to undergo subsequent chemotherapy and several had positive responses to treatment. One patient had a complete response to the epigenetic therapy, and one patient had a partial response. In all, seven patients remain alive, including two who began the therapy nearly 4 years ago.
Of the 45 patients enrolled in the study, all of whom received the epigenetic treatment, 19 were able to undergo subsequent chemotherapy and several had positive responses to treatment. One patient had a complete response to the epigenetic therapy, and one patient had a partial response. In all, seven patients remain alive, including two who began the therapy nearly 4 years ago.
The azacitidine/entinostat combination has been used successfully in patients with myelodysplastic syndrome and tested in leukemia patients with positive results. This study of the two drugs is believed to be the first to show anticancer activity in solid tumors—a pivotal finding, said the study researchers.
Non-small cell lung cancer accounts for nearly 80% of all lung cancer cases and is the main cancer-related cause of death. Azacitidine is a DNA methyltransferase inhibitor and entinostat inhibits histone deacetylation, a closely related process that also contributes to gene silencing. Laboratory studies of epigenetic therapy suggest that while the treatment does not kill cancer cells directly, it may reprogram malignant cells’ pattern of gene expression so that they lose their ability to grow uncontrollably.
Impressive Results in Patient Subset
 “This study looked at a combination of two drugs that target two different levels of epigenetic silencing to see if we could get synergy and gene re-expression, and with that, induce anticancer responses,” said Charles Rudin, MD, PhD, Professor of Oncology; Associate Director of Clinical Research at Johns Hopkins University Kimmel Cancer Center; and one of the lead investigators of the epigenetic study. “This therapy did not work in the majority of patients, but we did see a subset of patients who clearly benefited from the therapy, including some really impressive responses as well as some interesting periods of disease stabilization.”
“This study looked at a combination of two drugs that target two different levels of epigenetic silencing to see if we could get synergy and gene re-expression, and with that, induce anticancer responses,” said Charles Rudin, MD, PhD, Professor of Oncology; Associate Director of Clinical Research at Johns Hopkins University Kimmel Cancer Center; and one of the lead investigators of the epigenetic study. “This therapy did not work in the majority of patients, but we did see a subset of patients who clearly benefited from the therapy, including some really impressive responses as well as some interesting periods of disease stabilization.”
Another result of the study was the discovery of blood-based DNA methylation biomarkers of four genes: CDKN2A, CDH13, APC, and RASSF1A, which were identified as being strongly associated with disease recurrence and death in early-stage lung cancer and may allow physicians to predict which patients would benefit most from this type of treatment.
“What excited us perhaps more than anything else is when we looked at the methylation signature in four target genes that we think are important in lung cancer,” said Dr. Rudin. “The cohort of patients who had methylation of at least two of these targeted genes at baseline, and demethylated with therapy—suggesting that they were responding epigenetically to the treatment—actually did quite well and had a median survival of about 10.4 months, quite long for heavily pretreated patients. So we think we might have a biomarker for benefit from this therapy.”
Determining Prognostic and Diagnostic Biomarkers
 To test that theory, the study researchers are planning a follow-up trial to determine if the DNA methylation biomarkers are accurate predictors of who the best candidates are for this treatment. “You could imagine blood screening patients for the presence of these methylation markers and then treating patients with a single cycle of treatment to see whether they demonstrate a methylation response,” said Dr. Rudin.
To test that theory, the study researchers are planning a follow-up trial to determine if the DNA methylation biomarkers are accurate predictors of who the best candidates are for this treatment. “You could imagine blood screening patients for the presence of these methylation markers and then treating patients with a single cycle of treatment to see whether they demonstrate a methylation response,” said Dr. Rudin.
Another interesting finding from the study was that a number of trial participants had positive responses to subsequent chemotherapy following their epigenetic therapy, raising the possibility that epigenetic therapy primes the tumor for a better response to conventional chemotherapy.
“When you look at patients with advanced non–small cell lung cancer who have had previous treatments—some of our study patients had fourth- and fifth-line therapy by the time they got subsequent therapies—the response rates are generally very low, and they don’t see very good news with subsequent therapies,” said Stephen B. Baylin, MD, Professor and Deputy Director of the Johns Hopkins University Kimmel Cancer Center, and a co-principal investigator of the epigenetics study. “In this clinical trial, among the 34 patients who got more than one cycle of epigenetic therapy before they stopped, 20% had stable to really robust responses to their subsequent therapies, so that looks very unusual. It raises the hypothesis, but does not prove, that sensitization might have occurred.”
Future Research
To test the sensitization theory, the study researchers are developing another study and have applied to the NCI for approval to move ahead. “In the trial we are submitting to the NCI, the epigenetic therapy will start much earlier than in the trial we just completed. Patients will have had only one prior therapy, and then we will test them for sensitization. If this works, it will change the landscape of this disease, but we have to do the trials,” said Dr. Baylin.
The Johns Hopkins researchers have already launched a phase II adjuvant therapy trial to study the combination of azacitidine and entinostat in patients with early-stage lung cancers that have been surgically removed. ■
Disclosure: Dr. Rudin has been a consultant for Syndax. Dr. Baylin has been a consultant for, has research support from, and holds a patent licensed to MDxHealth.
Reference
1. Juergens RA, Wrangle J, Vendetti FP, et al: Combination epigenetic therapy has efficacy in patients with refractory advanced non–small cell lung cancer. Cancer Discovery 1(7):598-607, 2011.

