There’s no getting around it: the practice of oncology can be inherently stressful.
First, there’s the workload: compared to other medical specialists, oncologists see a larger number of patients and spend more time with them in face-to-face interactions. It’s not unusual for oncologists to work 60 hours per week.
Second, there’s the emotional toll, as oncologists often develop personal connections with patients, whom they might treat over many weeks, months, and even years. Over time, oncologists can become deeply invested in their patients’ health and well-being; when patients die, oncologists can experience classic symptoms of grief, including sadness and anxiety.
In addition to the long hours and the emotional toll, oncologists are called upon to participate in a host of professional activities, such as writing papers, giving presentations, and serving as chairs of committees. Not to mention keeping up with changes in reimbursement and practice management. Oh, and did you also want to spend time with your family and friends?
The responsibilities are endless and can all become too much for one person to handle. When competing demands reach a breaking point, oncologists are in danger of entering that fraught state—burnout.
Hallmark Signs of Burnout
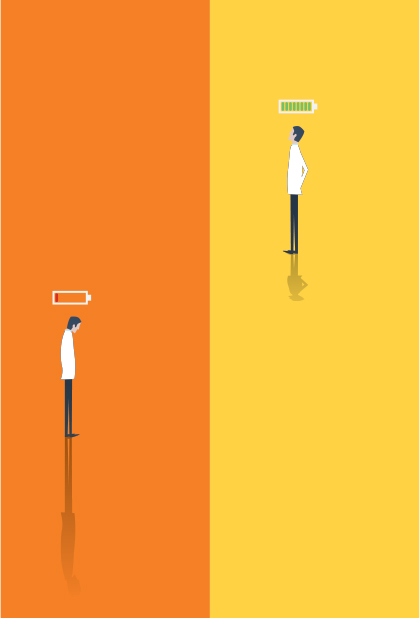
Burnout can manifest in many ways, but the three hallmark signs are depersonalization, exhaustion, and reduced personal accomplishment.
1) Depersonalization: Depersonalization occurs when the demands of work become overwhelming, pushing the individual to detach from the present moment and enter a mode of mechanistically going through the motions of life. In the context of medical practice, doctors who depersonalize run the risk of viewing patients as akin to tasks to check off on a to-do list and robotically fulfilling their duties.
2) Exhaustion: Exhaustion sets in when a doctor is nearing the point, or has reached the point, of having “maxed out” on the intellectual, physical, and emotional energy needed to effectively carry out the multiple demands of a busy clinic.
3) Reduced Personal Accomplishment: Doctors who feel reduced personal accomplishment doubt the meaning of their work, asking questions such as “Does what I do have any value?” and “Could it be I’m just not able to do a good job?”

We’ve become good at saying, ‘This person is burnt out,’ but we have a [long] way to go in establishing programs to prevent burnout.— Leora Horn, MD, MSc
Tweet this quote
Leora Horn, MD, MSc, a medical oncologist at Vanderbilt University with a strong interest in the study of burnout, explained how the thought “What’s it all for?” might resonate with both research and clinical oncologists.
“Let’s say you have someone who has spent years working in a lab, writing grants to pay her salary and keep the lab personnel funded, and she keeps getting negative results from her research. Or let’s say there’s a clinic where a physician is carrying out clinical research but finds he is perpetually getting negative findings from clinical trials and often loses patients he has come to care for,” Dr. Horn said. “Both the scientist and the clinician might just start to ask if there’s any point to doing what they do and feel that they just can’t go on with the work anymore.”
These situations aren’t just hypotheticals, she explained. “Recently I had an experience with a patient I had been treating for years. His disease progressed on his most recent therapy. When I started to talk about more treatment, he stopped me and said, ‘We fought a good battle, but I think it’s time for me to stop.’ My immediate reaction was to think, ‘What more could I have done for this patient?’ But then I had to remind myself that he had lived for 5 years with metastatic cancer. I had to remind myself to take a more balanced view of the work I do.”
Burnout Impacts Oncologists and Patients Too
According to an ASCO-sponsored study of burnout and career satisfaction among U.S. oncologists, 44.7% of surveyed oncologists reported feeling burned out on the emotional exhaustion and/or depersonalization domains. The main predictor of burnout was the amount of hours per week that doctors devoted to direct patient care. The survey results were published in a 2014 Journal of Clinical Oncology article, “Burnout and Career Satisfaction Among U.S. Oncologists,” coauthored by Dr. Horn.1
While burnout can have a large impact on oncologists’ quality of life, leading to anxiety, depression, and alcohol/substance use, it also has important professional consequences. Studies show that burnout adversely affects the quality of care oncologists are able to provide to patients. This connection between burnout and quality of care can be seen early on in a doctor’s career: Beginning in medical school, students experience a decline in empathy that has been tied to burnout and other forms of distress.2
Burnout also has important implications for the ongoing workforce shortage facing oncology—physicians experiencing burnout are more likely to reduce their work hours and/or pursue early retirement.
Steps to Combat Burnout
1) Acknowledge Your Feelings: According to Dr. Horn, the first step in addressing burnout is simply recognizing that you are experiencing it.
“The key is realizing that you need help,” she said. “Many people will push through or be too proud to ask for help, rather than recognizing that they are on a path that will decrease their own personal well-being and that of their patients. Once you stop, and say, ‘Okay, I’ve reached my limit,’ or ‘My passion for my job has dimmed,’ you can start asking for help and thinking of creative ways to revive your energy and become excited about work again.”
2) Grieve the Loss of Your Patients: Oncologists should know it is healthy and okay to take time to grieve in a way that makes sense for them personally. The rationale for dedicating time to reflect upon loss was eloquently stated by Jimmie Holland, MD, a psychiatrist at Memorial Sloan Kettering Cancer Center, in a 2006 Journal of Oncology Practice article, “Managing Stress and Burnout in Oncology”3:
“In terms of your own survival, it is important to recognize that the death of some patients can affect you much more deeply than others. You can often recognize a resemblance in appearance or age or temperament of the patient that reminded you of someone in your past, and you can see why the death affects you so much more deeply.”
3) Focus on Your Well-Being: Burnout can arise when tunnel vision sets in, narrowing your scope and reducing all of life to “work, work, work.” If you find yourself in this zone, take steps to widen your perspective:
Set aside time for activities outside of work that bring you joy, whether that means doing yoga, cooking, watching a game, or going for a run. For some people, writing an academic paper or attending a conference is an antidote to stress—this is okay, as long as it allows you to break out of a work-only mode.
Seek out sources of emotional support, whether a professional therapist, friends, or family.
Practice the pillars of self-care: adequate sleep, good nutrition, and regular exercise.
Take a vacation. Dr. Horn suggests taking time off every 3 to 4 months to spend time doing what you like, allowing you to come back newly energized and excited about your work. “Whether we want to believe it or not, we’re all replaceable. You always can leave, and rest assured, the work will still be there when you come back,” she said.
4) Manage Your Time and Respect Your Own Limits: It can be difficult to say no when colleagues and patients ask for more of your time. One way to ensure you’ll have some free moments is to block off your calendar for times that cannot be used for meetings or work-related activities.
“I think it’s important that on days when I’m not in clinic, I don’t schedule meetings late into the day. This way, I can be home for dinner and bedtime, so I get to see my kids, which I don’t always get to do on clinic days or when I’m on in patient service,” Dr. Horn said. “Blocking time off applies to other areas of life as well, for example, a singing class you enjoy or a reading group.”
If you’re finding that you’re truly treading water when it comes to time management, consider reducing the number of patients you see or the number of new patients you take on, if possible. Recognizing that patient overload is often a problem for doctors, many practices are delegating work to advanced practice providers such as physician assistants and nurse practitioners.
5) Take Advantage of Institutional Services: There are times when burnout will be felt acutely, despite a doctor’s best efforts to take vacations, find social support, and make time for reenergizing activities. At those times, find out if your practice or institution has an Employee Assistance Program, which may offer support staff, programming, and education sessions to help you deal with burnout. For example, the Mayo Clinic created a Listen-Act-Develop model, which includes a forum in which doctors can discuss sources of stress and brainstorm how to have more control over their schedules.
6) Prevention Is the Goal: Dr. Horn said that, ultimately, physician associations and institutions are good at defining and recognizing burnout but not as effective at helping to prevent burnout it before it happens.
“We’ve become good at saying, ‘This person is burnt out,’ but we have a [long] way to go in establishing programs to prevent burnout,” she explained. “Wouldn’t it be great if we had a tool that allowed oncologists to take a personal inventory, whether every 2 months or twice a year, that would allow them to think, ‘Hey, how am I doing?’” ■
References
3. Managing stress and burnout in oncology. J Oncol Pract 2:130-131, 2006.
Originally printed in ASCO Connection. © American Society of Clinical Oncology. “An Introduction to Recognizing and Managing Professional Burnout.” ASCO Connection, January 2017: 46-47. All rights reserved.

