Following a priority review process for orphan diseases, ruxolitinb (Jakafi) recently became the first drug to receive FDA approval for the treatment of intermediate- and high-risk myelofibrosis. Discovery in 2004 of the JAK2V617F mutation in a significant proportion of patients with BCR-ABL1–negative chronic myeloproliferative neoplasms spurred the development of several small-molecule JAK inhibitors. Ruxolitinib was first out of the gate, with time from phase I testing to drug approval of approximately 4 years.
Myelofibrosis can develop de novo (primary myelofibrosis), or following fibrotic transformation of polycythemia vera or essential thrombocythemia. Current drug therapy for myelofibrosis is suboptimal. Hydroxyurea is widely used to control symptomatic splenomegaly and leukocytosis/thrombocytosis, but is ineffective in advanced disease stages; it does not improve constitutional symptoms (fever, night sweats, bone pain, cachexia, weight loss) and may exacerbate anemia or other cytopenias. Anemia responses are relatively infrequent (10%–20%) and not durable with use of erythropoiesis-stimulating agents, androgens, low-dose thalidomide (Thalomid), danazol, and corticosteroids. Given that the median age at diagnosis in myelofibrosis is 65 years, few patients are eligible for allogeneic stem cell transplant.
Clinical Trial Data Supporting Drug Approval
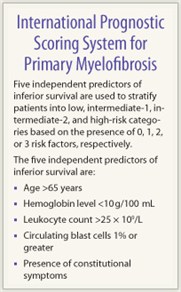
 Two randomized controlled trials were conducted: (1) the Controlled Myelofibrosis Study with Oral Janus-associated Kinase (JAK) Inhibitor Treatment-I (COMFORT-I), a randomized (1:1), double-blind study comparing ruxolitinib to placebo; and (2) COMFORT-II, a randomized (2:1) open-label study, comparing ruxolitinib to best available therapy (no therapy or best available therapy was selected by the investigator on a case-by-case basis). Key eligibility criteria included patients with intermediate-2 or high-risk primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis who were JAK inhibitor therapy–naive, with adequate organ function and hematologic reserve (minimum platelet count = 100 × 109/L).
Two randomized controlled trials were conducted: (1) the Controlled Myelofibrosis Study with Oral Janus-associated Kinase (JAK) Inhibitor Treatment-I (COMFORT-I), a randomized (1:1), double-blind study comparing ruxolitinib to placebo; and (2) COMFORT-II, a randomized (2:1) open-label study, comparing ruxolitinib to best available therapy (no therapy or best available therapy was selected by the investigator on a case-by-case basis). Key eligibility criteria included patients with intermediate-2 or high-risk primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis who were JAK inhibitor therapy–naive, with adequate organ function and hematologic reserve (minimum platelet count = 100 × 109/L).
The primary endpoint was the proportion of patients with ≥ 35% reduction in spleen volume at week 24 and 48 of therapy (COMFORT-I and COMFORT-II, respectively), assessed by blinded review of spleen MRI or CT. The key secondary endpoints for COMFORT-I were durability of spleen response and changes in symptom burden. The ruxolitinib dose was 15 or 20 mg twice daily, depending on a baseline platelet count of 100 to 200 × 109/L or > 200 × 109/L, respectively.
COMFORT-I Results
 In COMFORT-I, 309 patients were randomly assigned—155 to ruxolitinib and 154 to placebo. At week 24, 65 patients (41.9%) met the primary endpoint in the ruxolitinib arm vs 1 patient (0.7%) in the placebo arm (P < .0001). At this time point, 68 patients (45.9%) vs 8 patients (5.3%) achieved a minimum 50% reduction in the total symptom score in the ruxolitinib and placebo arms (P < .0001).
In COMFORT-I, 309 patients were randomly assigned—155 to ruxolitinib and 154 to placebo. At week 24, 65 patients (41.9%) met the primary endpoint in the ruxolitinib arm vs 1 patient (0.7%) in the placebo arm (P < .0001). At this time point, 68 patients (45.9%) vs 8 patients (5.3%) achieved a minimum 50% reduction in the total symptom score in the ruxolitinib and placebo arms (P < .0001).
The most frequent adverse reactions (overall/grade 3 or 4 for ruxolitinib vs placebo) were thrombocytopenia (69.7%/12.9% vs 30.5%/1.3%), anemia (96.1%/45.2% vs 86.8/19.2%), neutropenia (18.7%/7.1% vs 4%/2%), bruising (23.2%/0.6% vs 14.6%/0%), dizziness (18.1%/0.6% vs 7.3%/0%) and headache (14.8%/0% vs 5.3%/0%).
In the initial report (median follow-up = 32.2 weeks), there was no significant survival difference in the two study arms; with longer follow (median ~1 year), significantly fewer deaths were noted in the ruxolitinib arm (n = 13) compared to the placebo arm (n = 24), with a hazard ratio of 0.5 (P = .04).
COMFORT-II Results
In COMFORT-II, 219 patients were randomly assigned—146 to ruxolitinib and 73 to best available therapy (including hydroxyurea in 47% and glucocorticoids in 16%). At week 48, 41 patients (28.5%) vs 0 patients met the primary endpoint in the ruxolitinib and best available therapy arms (P < .0001). At week 24, the corresponding response rates were 31.9% vs 0% (P < .0001). The most frequent hematologic adverse reactions (overall/grade 3 or 4 for ruxolitinib vs best available therapy) were thrombocytopenia (44.5%/7.5% vs 9.6%/4.1%) and anemia (40.4%/11% vs 12.3/4.1%). Nonhematologic adverse reactions of any grade (ruxolitinib vs best available therapy) included diarrhea (24% vs 11%) and peripheral edema (21.9% vs 26%). There was no significant difference in the number of deaths between the two arms in this study.
Risk-benefit Considerations
Patients with intermediate-2 and high-risk myelofibrosis have a median survival of about 3.6 and 1.8 years, respectively. In this category, the ideal patient for ruxolitinib therapy has symptomatic splenomegaly and/or significant constitutional symptoms with well-preserved blood counts, and is not a candidate for early allogeneic stem cell transplant based on the presence of very high-risk disease features. The risk-benefit ratio is less optimal for the patient whose main disease feature is severe anemia, with or without other concurrent cytopenias. Anemia responses are relatively infrequent (10%–20% based on phase I data) and are counterbalanced by a relatively high incidence of treatment-emergent cytopenias.1
 The current studies are not adequately powered to assess for survival benefit; further, the COMFORT-II study, which more closely reflects the “real-world” scenario wherein patients with advanced, symptomatic myelofibrosis receive “best available therapy” (rather than no therapy/placebo, as in the COMFORT-I control arm) showed no survival benefit for ruxolitinib. Consequently, any claims to the contrary, particularly if supported by comparison with a historical cohort, are potentially misleading, and should not be used as a basis for counseling patients regarding this issue.
The current studies are not adequately powered to assess for survival benefit; further, the COMFORT-II study, which more closely reflects the “real-world” scenario wherein patients with advanced, symptomatic myelofibrosis receive “best available therapy” (rather than no therapy/placebo, as in the COMFORT-I control arm) showed no survival benefit for ruxolitinib. Consequently, any claims to the contrary, particularly if supported by comparison with a historical cohort, are potentially misleading, and should not be used as a basis for counseling patients regarding this issue.
Patients with intermediate-1–risk disease have a median survival of about 7.8 years. In such patients with symptomatic splenomegaly or constitutional symptoms (eg. severe pruritus) that are not responsive to conventional measures, ruxolitinib treatment may be cautiously considered, but only after a full and transparent discussion regarding potential risks and benefits. Patients should be informed about the lack of data regarding long-term treatment-related toxicities and the risk of rare serious adverse events.
Low-risk myelofibrosis patients have a median survival of about 17.5 years and are generally not candidates for ruxolitinib treatment, with rare exception, given that they risk more harm (eg. anemia, thrombocytopenia) than good from such therapy.
Drug Discontinuation
Patients and physicians should be informed regarding what to potentially expect when discontinuing JAK inhibitors. Relapse of disease symptoms occurs virtually universally in this setting. In the case of ruxolitinib, symptoms recur within days and in some patients may be associated with hyperacute features (“ruxolitinib withdrawal syndrome,” which may be characterized by rapid spleen regrowth with splenic infarction, or cardiopulmonary distress).2,3 Patients should be closely monitored during the drug discontinuation process and follow a tapering schedule rather than abrupt cessation.
Long-term Findings
With respect to response durability and long-term toxicity, only limited long-term data are available, so just a preliminary analysis is possible. Phase I data have been previously reported;1 recently, long-term data were separately analyzed for the Mayo Clinic (n = 51) and MD Anderson Cancer Center (n = 107) cohorts. Treatment discontinuation rates at the Mayo Clinic at 1, 2, and 3 years were 51%, 72%, and 89%; discontinuations were largely secondary to loss of response and/or toxicity. At MD Anderson, 54% of patients continue on treatment after a median follow-up of 32 months. At the time of drug approval, 75% and 67% of patients who achieved a ≥ 35% reduction in spleen volume on COMFORT-I and COMFORT-II, respectively, maintained that response.
Cytopenias are generally managed with dose reductions; this can be problematic in that it may lead to loss of response and, consequently, treatment discontinuation. In some cases, drug is discontinued based on patient preference if treatment benefit is considered too modest to justify continued treatment, particularly when a new requirement for red cell transfusions develops.
Mechanisms of Action
 There are two potential mechanisms of ruxolitinib in myelofibrosis: (1) inhibition of constitutively active JAK-STAT signaling (that develops as a consequence of JAK2 mutations or other phenocopy mutations such as MPL, LNK and CBL), with direct inhibition of clonal myeloproliferation (accordingly, presence or absence of JAK2V617 does not influence the therapeutic response to ruxolitinib); and/or (2) downregulation of proinflammatory cytokines such as interleukin-6 and tumor necrosis factor-α, via ruxolitinib’s JAK1 inhibitory properties. Suppression of the secondary, paraneoplastic, chronic inflammatory state in myelofibrosis may improve constitutional symptoms and indirectly control the underlying clonal myeloproliferation.
There are two potential mechanisms of ruxolitinib in myelofibrosis: (1) inhibition of constitutively active JAK-STAT signaling (that develops as a consequence of JAK2 mutations or other phenocopy mutations such as MPL, LNK and CBL), with direct inhibition of clonal myeloproliferation (accordingly, presence or absence of JAK2V617 does not influence the therapeutic response to ruxolitinib); and/or (2) downregulation of proinflammatory cytokines such as interleukin-6 and tumor necrosis factor-α, via ruxolitinib’s JAK1 inhibitory properties. Suppression of the secondary, paraneoplastic, chronic inflammatory state in myelofibrosis may improve constitutional symptoms and indirectly control the underlying clonal myeloproliferation.
Current data favor the latter as the dominant mechanism for ruxolitinib’s activity in myelofibrosis. Specifically, phase I data show potent suppression of cytokines, but a modest and variable effect on circulating JAK2V617F allele burden. ■
Disclosure: Dr. Pardanani has served as Principal Investigator/Co-investigator for clinical trials that received institutional support (free drug and funding) from Incyte, sanofi-aventis, TargeGen, YM BioSciences, Cytopia, Bristol-Myers Squibb, Celgene, and Novartis. TargeGen and Cytopia have also provided support for laboratory studies relevant to clinical trials. Dr Tefferi has served as Principal Investigator/coinvestigator for clinical trials that received institutional support (free drug and funds) from Incyte, Sanofi-Aventis, TargeGen, YM BioSciences, Cytopia, Bristol-Myers Squibb, Celgene, and Novartis. TargeGen, Cytopia, and YM BioSciences have also provided support for laboratory studies relevant to clinical trials.
References
1. Verstovsek S, Kantarjian H, Mesa R, et al: Safety and efficacy of INCB018424, a JAK1 and JAK2 inhibitor, in myelofibrosis. N Engl J Med 363:1117-1127, 2010.
2. Tefferi A, Litzow MR, Pardanani A: Long-term outcome of treatment with ruxolitinib in myelofibrosis. N Engl J Med 365:1455-1457, 2011.
3. Tefferi A, Pardanani A: Serious adverse events during ruxolitinib treatment discontinuation in patients with myelofibrosis. Mayo Clin Proc 86:1188-1191, 2011.
Dr. Pardanani is Assistant Professor of Medicine, Division of Hematology, Department of Medicine, Mayo Clinic, Rochester, Minnesota.

