In the phase III SOPHIA trial of 536 heavily pretreated patients with HER2-positive metastatic breast cancer, the novel anti-HER2 antibody margetuximab plus chemotherapy led to significant improvements in progression-free survival, response, and clinical benefit compared with trastuzumab/chemotherapy.1 The benefits were enhanced in patients with low-affinity CD16A-158F -genotypes.

This is the first prospective analysis of the CD16A genotype as a predictor of efficacy from anti-HER2 therapy.— Hope S. Rugo, MD
Tweet this quote
“This is the first prospective analysis of the CD16A genotype as a predictor of efficacy from anti-HER2 therapy,” according to Hope S. Rugo, MD, of the University of California San Francisco Helen Diller Family Comprehensive Cancer Center, who presented the primary progression-free survival analysis of SOPHIA at the 2019 ASCO Annual Meeting. “Although the 1-month absolute benefit in progression-free survival has slight clinical relevance, the benefit was enhanced in patients who carry at least one F allele,” she added.
Controversy exists about the role of CD16A polymorphisms on the efficacy of trastuzumab, Dr. Rugo noted. Two retrospective studies of patients with HER2-positive early and metastatic breast cancers suggested that those who carry the low-affinity F allele have shorter progression-free survival and lower overall response rates with trastuzumab than those who are homozygous for the higher-affinity V allele.
The current standard of care for HER2-positive metastatic breast cancer is trastuzumab plus pertuzumab and chemotherapy in the first-line setting and trastuzumab emtansine (T-DM1) in the second line. After patients experience disease progression on these treatments, there is no recognized standard of care, although continued anti-HER2 therapy is generally preferred in combination with chemotherapy, Dr. Rugo commented.
Unique Characteristic of Margetuximab
Margetuximab is an Fcγ-engineered antibody designed to activate an immune response. Previous preclinical and phase I studies showed that margetuximab does, indeed, enhance innate immunity and HER2-specific adaptive immunity.
Margetuximab has similar HER2-binding and antiproliferative effects as trastuzumab. By contrast, however, its Fcγ region is engineered to increase affinity for both alleles of the activating Fc receptor (FcgR)—CD16A—and to decrease affinity for the inhibitory FcgR, CD32B. The low-affinity CD16A-158F allele (which is seen in about 85% of the population) has been associated with diminished clinical response to trastuzumab, explained Dr. Rugo.
“The hypothesis of SOPHIA was that margetuximab would have greater benefit than trastuzumab in the lower-binding CD16A-158F carriers, as it has increased affinity for CD16A-158F over trastuzumab,” she said.
SOPHIA Details
The open-label phase III SOPHIA trial enrolled 536 patients with HER2-positive metastatic breast cancer who had been treated with at least two prior lines of anti-HER2 therapy, including pertuzumab, and one to three prior lines in the metastatic setting. Patients were randomly assigned 1:1 to margetuximab (15 mg/kg intravenously every 3 weeks) or trastuzumab (6 mg/kg [8-mg/kg loading dose]). In both arms, anti-HER2 therapy was given with physician’s choice of chemotherapy (capecitabine, eribulin, gemcitabine, or vinorelbine). The primary endpoints were progression-free and overall survival, by central blinded assessment.
All patients had received trastuzumab and pertuzumab, and more than 90% had also received T-DM1. Almost all had received a taxane, more than 40% had received an anthracycline, and almost half had received an endocrine agent.
Risk of Disease Progression Reduced
In theprogression-free analysis of the intent-to-treat population, the risk of disease progression was reduced by 24% in the central blinded review (primary endpoint), based on a median progression-free survival of 5.8 months with margetuximab/chemotherapy vs 4.9 months with trastuzumab chemotherapy (hazard ratio [HR] = 0.76; P = .033). Risk reduction was 30% according to investigator assessment (secondary endpoint).
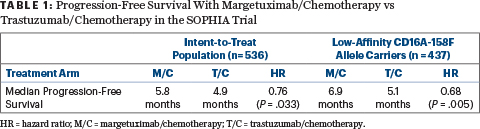
In the planned exploratory analysis by CD16A genotype, the benefit was enhanced in patients with low-affinity CD16A genotypes containing a 158F allele, whose disease progression was reduced by 32% (Table 1).
The objective response rate was higher with margetuximab/chemotherapy than with trastuzumab/chemotherapy, 22.1% vs 16.0% (P = .060), as was the clinical benefit rate, 36.6% vs 24.8% (P = .003).
Analysis by CD16A Genotype
Within theCD16A-158F genotype, important differences were also observed according to alleles. The median progression-free survival with margetuximab/chemotherapy versus trastuzumab/chemotherapy in the various allele subsets follows:
- FF or FV genotype: 6.9 vs 5.1 months (HR = 0.68; P = .005)
- VV genotype: 4.8 vs 5.6 months (HR = 1.78; P = .110)
- FF genotype (n = 192): 8.2 vs 5.6 months (HR = 0.69; P = .080)
- FV genotype: 6.3 vs 4.3 months (HR = 0.71; P = .055).
“In this preplanned exploratory analysis, we saw that the alleles for CD16A made a difference in the efficacy of margetuximab/chemotherapy,” Dr. Rugo said. “In patients who were homozygous for the high-affinity VV allele, the effect of margetuximab and trastuzumab was relatively similar, but in the 85% who carry at least one F allele, the progression-free benefit was enhanced, and it was further enhanced in patients who were homozygous for the F allele, who had a greater difference in progression-free survival.”
Margetuximab and Chemotherapy in Breast Cancer
- In the phase III SOPHIA trial, the novel anti-HER2 antibody margetuximab plus chemotherapy significantly improved progression-free survival over trastuzumab/chemotherapy in heavily pretreated patients with metastatic breast cancer.
- The risk of disease progression was reduced by 24% in the central blinded review (primary endpoint) and by 30% according to investigator assessment (secondary endpoint).
- In the planned exploratory analysis by CD16A genotype, the benefit was enhanced in patients with low-affinity CD16A genotypes containing a 158F allele, whose disease progression was reduced by 32%.
The interim overall survival analysis similarly showed that most benefit occurred in CD16A-158F carriers. In the whole population, the median overall survival was 18.9 months with margetuximab and 17.2 months with trastuzumab (HR = 0.95); however, in the carriers, it was 23.6 months and 16.9 months, respectively (HR = 0.82), although this was not yet statistically significant. “Of course,” she commented, “this isn’t ready for statistical significance, but it’s an intriguing finding.”
“The most interesting finding was in the interim analysis, where only 40% of the overall survival events needed for assessment had occurred. Despite this, there was a marked and clinically significant difference in overall survival in the F allele carriers receiving margetuximab. This needs to be confirmed in the second interim analysis, which is expected later this year,” Dr. Rugo told The ASCO Post.
Safety profiles were comparable, with grade ≥ 3 adverse events and serious adverse events occurring in 52% and 15% of the margetuximab arm, respectively, vs 48% and 17% receiving trastuzu-mab; treatment discontinuation rates were about 3% in each arm. Infusion-related reactions were more common with margetuximab, but just 1.5% were grade ≥ 2 and were managed with premedication.
The next milestone will be the second interim overall survival analysis, expected in late 2019, Dr. Rugo indicated. ■
DISCLOSURE: Dr. Rugo has received institutional research funding from Daiichi Sankyo, Eisai, Genentech, Immunomedics, Lilly, MacroGenics, Merck, Novartis, OBI Pharma, Odonate Therapeutics, Pfizer, and Seattle Genetics as well as received travel expenses from Amgen, Mylan, Novartis, OBI Pharma, Pfizer, Puma Biotechnology, Roche/Genentech, and Sanofi.
REFERENCE
1. Rugo HS, et al: SOPHIA primary analysis. 2019 ASCO Annual Meeting. Abstract 1000. Presented June 4, 2019.


