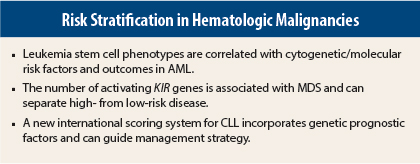
Refinements in the classification and risk stratification for leukemia and myelodysplastic syndromes were reported by three different investigators at the 2015 ASCO Annual Meeting. The first study showed that leukemia stem cell phenotypes are associated with outcomes in acute myeloid leukemia (AML).1 The second study suggested that the number of activating killer-cell immunoglobulin-like receptor (KIR) genes is associated with the development of myelodysplastic syndromes (MDS), with the potential to be used for risk stratification.2 The third study highlighted an updated international scoring system for chronic lymphocytic leukemia (CLL) that incorporates genetic risk factors.3
Leukemia Stem Cells in AML
Three distinct, mutually exclusive subtypes of leukemia stem cells recently identified are correlated with both specific cytogenetic/molecular risk factors and response and outcomes. These leukemia stem cell phenotypes are based on CD34, CD38, and aldehyde dehydrogenase (ALDH) expression as follows:
- CD34-negative
- CD34-positive, CD38-negative, ALDH-intermediate (most common subtype)
- CD34-positive, CD38-negative, ALDH-high
In AML, remission does not equal cure. “Current prognostic factors [cytogenetics] are limited, and it can take over a week to get test results, which is not good for such an explosive disease. Grouping AML patients according to leukemia stem cell phenotype may permit rapid risk stratification without identifying molecular/cytogenetic features,” stated lead author Jonathan Gerber, MD, of Levine Cancer Institute, Charlotte, North Carolina.
The phase II NCTG0143880 trial was based on tissue samples available for 98 of 165 newly diagnosed patients with poor-risk disease or those who had unfavorable cytogenetic AML. Forty percent of patients harbored adverse cytogenetics. Fluorescent in situ hybridization and/or polymerase chain reaction were used to analyze the cell populations for leukemia-specific abnormalities, and leukemia stem cell phenotypes were found to correlate with specific cytogenetic and molecular risk factors.
Poor-risk cytogenetics and/or FLT3/ITD mutations were uncommon in the CD34-negative phenotype (4 of 22, 18%) and the ALDH-intermediate phenotype (17 of 43, 35%) but were found in 28 of 33 patients (85%) in the ALDH-high group (P < .001).
NPM1 mutations, associated with a good prognosis, were found in 14 (64%) of the CD34-negative group vs 6 (14%) of the ALDH-intermediate and 2 (6%) of the ALDH-high group (P < .001).
Outcomes differed according to leukemia stem cell phenotype. The rate of complete remission was 86% in the CD34-negative group; complete remission was 67% in the ALDH-intermediate group and 45% in the ALDH-high group. Median event-free survival was 13 months, 11.3 months, and 2.2 months for the three phenotypes, respectively. The rate of 2-year event-free survival was 46%, 26%, and 0% for the three phenotypes, respectively.
Overall survival was not yet reached in the CD34-negative patients; overall survival was 18.7 months in the ALDH-intermediate group and 2.2 months in the ALDH-high group.
“Risk stratification according to leukemia stem cell phenotype makes it possible to divert high-risk (ALDH-high) patients to earlier novel forms of therapy and transplant. These patients don’t do well on conventional chemotherapy,” Dr. Gerber said.
Two patterns were evident in patients in complete remission: normal with no ALDH and no leukemia stem cells and minimal residual disease with persistent ALDH expression. The presence of minimal residual disease predicted prognosis; six of seven patients with minimal residual disease relapsed. All patients with no evidence of minimal residual disease remained in clinical remission more than 4 years later.4
Activating KIR Genes in MDS
The number of activating KIR genes (killer-cell immunoglobulin-like receptor genes) is related to the risk of developing MDS and categorizing patients with MDS as high risk vs low risk. However, the number of KIR genes is not related to overall survival, according to a preliminary case-control study.
The study population included 180 patients with MDS; of them, 120 were at low risk and 60 were at high risk. Patients with MDS were compared with 117 healthy donor controls. The age distribution was similar between both groups; more than 80% were older than age 60. DNA samples were collected in both cases and controls and analyzed for activating KIR genes using polymerase chain reaction.
Patients with high-risk MDS had significantly lower numbers of activating KIR genes than did patients with low-risk MDS (P = .009) and healthy controls (P = .00001). Patients with low-risk MDS also had significantly lower numbers of activating KIR genes than did controls (P = .04). Moreover, the inheritance of each additional activating KIR gene had a protective effect against the development of high-risk MDS (P < .001).
“This study provides novel insights concerning the pathogenesis of MDS in adults. These results suggest that inheritance of a higher number of activating KIR genes is protective against MDS and that once the disease develops, harboring a lower number of KIR genes is associated with higher-risk disease,” said lead author May Daher, MD, of The University of Texas MD Anderson Cancer Center, Houston.
The major concern with MDS is the potential to evolve to AML, which is difficult to treat, and occurs in about 20% of patients with MDS. In this study, transformation to AML occurred in 12% of low-risk patients vs 20% of the high-risk group.
New CLL–IPI Scoring System
MDS can be risk stratified using the International Prognostic Scoring System. The CLL–IPI International Working Group has developed the International Prognostic Index for patients with CLL (CLL–IPI), which combines genetic risk factors with clinical stage, age, and beta-2 microglobulin (B2M) into a clinically applicable prognostic score. Moreover, the CLL–IPI discriminates between prognostic groups and can inform treatment decisions.
“The traditional staging systems developed more than 30 years ago for CLL do not discriminate enough anymore. There are newly discovered prognostic markers, but no system integrates all these markers. We report on an international effort to develop a comprehensive score,” said Nadine Kutsch, MD, on behalf of the International CLL–IPI working group. Dr. Kutsch is from the Center for Integrated Oncology Cologne Bonn, University of Cologne, Germany.
The full analysis set relied on data from eight phase III trials in Europe that included 3,472 treatment-naive patients in various stages of CLL. The median age was 61 years, the median observation time was 80 months, and 89% of patients have received treatment so far. The full analysis set was randomly divided into training (n = 2,308) and internal validation datasets (n = 1,164). The new CLL–IPI was externally validated in a third dataset comprising prospectively collected data from 848 patients treated at the Mayo Clinic, Rochester, Minnesota; the median age of patients was 62 years, and 39% have received treatment so far.
The different analysis steps identified five independent predictors for overall survival, and the parameters from the regression model were used to grade the factors according to their individual impact: TP53 (17p) del/mut = 4, IGHV unmutated = 2, B2M > 3.5 mg/L = 2, clinical stage Binet B/C or Rai I–IV = 1, age > 65 years = 1.
A prognostic score was developed ranging from 0–10, and four different risk groups were derived: prognostic score of 0–1, low risk; prognostic score of 2–3, intermediate risk; prognostic score of 4–6, high risk; and prognostic score of 7–10, very high risk.
These four risk groups, respectively, had different overall survival rates at 5 years: 93%, 79%, 64%, and 23% (P < .001). This model was confirmed on the internal validation dataset and then on the Mayo set, with 5-year overall survival rates of 94%, 91%, 68%, and 21%, for the low to very-high-risk groups, respectively.
The CLL–IPI system is clinically applicable. Low-risk patients should be managed with “watch and wait.” Intermediate-risk patients should not be treated unless they are symptomatic. High-risk patients should be treated, unless they are asymptomatic. Very-high-risk patients should be treated with experimental approaches. ■
Disclosure: Dr. Kutsch has received honoraria from Janssen and Grifols and travel grants from Mundipharma. Drs. Gerber and Daher reported no potential conflicts of interest.
References
1. Gerber JM, Zeidner JF, Morse S, et al: Correlation of acute myeloid leukemia stem cell phenotype with cytogenetic/molecular features and prognosis. 2015 ASCO Annual Meeting. Abstract 7000.
2. Daher M, Sobieski C, Marin D, et al: Association between KIR genes and risk of MDS. 2015 ASCO Annual Meeting. Abstract 7001.
3. Kutsch N, Bahlo J, Byrd JC, et al: The International Prognostic Index for patients with CLL (CLL-IPI). 2015 ASCO Annual Meeting. Abstract 7002.
4. Gerber JM, Smith BD, Ngwang B, et al: A clinically relevant population of leukemic CD34+CD38– cells in acute myeloid leukemia. Blood 119:3571-3577, 2012.