ESR1 mutations are known to confer resistance to endocrine therapy in the metastatic breast cancer setting. These mutations herald a poor prognosis, so their clearance early in the treatment course may greatly reduce the risk of recurrence, according to the early results of the prospective phase III PADA-1 trial, reported during the ASCO20 Virtual Scientific Program.1
The study involved 1,017 patients with metastatic, hormonally sensitive breast cancer treated in the first-line setting with an aromatase inhibitor plus palbociclib. It found that patients with ESR1 mutations at baseline, compared with those who had ESR1 wild-type tumors, had double the odds of disease progression. However, if those mutations were cleared early during treatment, this risk diminished to roughly that of their wild-type peers. Of note, PRADA-1 also found the mutation was more than twice as prevalent—7% vs 3%—among patients who received an aromatase inhibitor in the adjuvant setting.

“ESR1 mutation screening before starting first-line treatment with an aromatase inhibitor plus palbociclib could be considered for patients at higher risk of ESR1 mutations.”— François-Clément Bidard, MD, PhD
Tweet this quote
“ESR1 mutation screening before starting first-line treatment with an aromatase inhibitor plus palbociclib could be considered for patients at higher risk of ESR1 mutations,” stated lead investigator François-Clément Bidard, MD, PhD, of the Institut Curie, Paris.
Study Rationale
The question of which is the best endocrine partner to cyclin-dependent kinase 4/6 (CDK4/6) inhibitors as first-line treatment has remained unanswered. ESR1 mutations are detected in between 1% and 5% of patients upon first relapse but in up to 40% of patients who become resistant to an aromatase inhibitor.
“ESR1 mutations might be of paramount importance, as they confer resistance to aromatase inhibitors but not to selective estrogen receptor degraders such as fulvestrant,” Dr. Bidard noted.
In patients treated with first-line palbociclib plus an aromatase inhibitor, the PADA-1 trial determined the rate of ESR1 mutations at study inclusion and shortly after therapy was initiated as well as looked at the association between mutation and prognosis. PADA-1 also evaluated the utility of monitoring the onset of ESR1 mutations in cell-free DNA. Dr. Bidard presented the early results for the first part of this study.
PADA-1 Details
This trial included 1,017 patients with estrogen receptor–positive, HER2-negative, metastatic breast cancer who had received no prior therapy for metastatic disease and had no overt resistance to aromatase inhibitors. Sensitivity was assumed based on no prior treatment with an aromatase inhibitor or a disease-free interval of more than 12 months from adjuvant treatment with one.
Patients had cell-free DNA tested for ESR1 mutations at inclusion and during treatment with an aromatase inhibitor plus palbociclib (step 1). Some 565 patients developed progressive disease and were eliminated from the study. For 135 patients, an emerging ESR1 mutation was detected, although disease was not progressing; these patients were randomly assigned to continue the same treatment or switch to fulvestrant plus palbociclib (step 2, n = 135). (These data will be reported at a later date.)
KEY POINTS
- The prospective phase III PADA-1 trial is evaluating the prognostic impact of ESR1 mutations in the first-line metastatic setting of estrogen receptor–positive/HER2-negative breast cancer treated with an aromatase inhibitor and palbociclib.
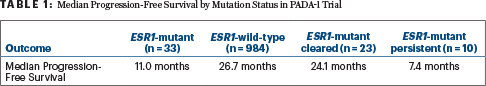
- The presence of ESR1 mutation at baseline heralded a worse prognosis: median progression-free survival was 11.0 months for mutation-positive patients but 26.7 months for patients with wild-type disease (hazard ratio = 2.3).
- Clearance of the mutation after 1 month of treatment improved the prognosis of patients initially ESR1-positive, whose median progression-free survival was 24.1 months, compared with 7.4 months for patients who did not clear the mutation.
- Patients who received an aromatase inhibitor as adjuvant treatment as well were twice as likely to have an ESR1 mutation as those who did not.
At inclusion, testing identified 33 patients with mutations (3.2%). The presence of this mutation at baseline was associated with prior exposure to an aromatase inhibitor in the adjuvant setting, with a prevalence of 7.1% among patients with at least 3 years of adjuvant treatment vs 3.2% in the overall population (odds ratio [OR] = 3.0). ESR1 mutations were also more likely among patients with bone metastases (4.0%; OR = 3.4) and among postmenopausal women (4.1%; OR = 5.4).
Worse Prognosis Associated With ESR1 Mutation
At a median follow-up of 21.2 months, median progression-free survival for the 33 mutation-positive patients was 11.0 months, but it was 26.7 months for patients with ESR1 wild-type disease (HR = 2.3; P < .001).
“No multivariate analysis was done, as many patients are still being followed in step 1,” Dr. Bidard explained. “However, a sensitivity analysis found no impact of the type of adjuvant endocrine therapy on progression-free survival.”
Clearance of ESR1 Mutations
For 23 of the 33 patients (69%), ESR1 mutations were cleared after 4 weeks of treatment. However, 15 of these patients experienced a later “resurgence” of the mutation. A smaller subgroup of 10 patients experienced no mutational clearance at 4 weeks.
In addition, clearance of ESR1 mutations heralded a better prognosis. The median progression-free survival was 24.1 months in the cleared group vs 7.4 months in those with still-detectable ESR1 mutations (Table 1).
In closing, Dr. Bidard said ESR1 mutation at baseline is a prognostic marker for patients treated with an aromatase inhibitor and palbociclib. However, “both the 11-month median progression-free survival in patients with ESR1-mutated disease and the frequent clearance of the mutation after one cycle suggest an aromatase inhibitor plus palbociclib retains some activity despite the ESR1 mutation,” he commented.
New oral selective estrogen receptor degraders are of increasing interest as a means of further improving the outcomes of patients with ESR1 mutations, said Dr. Bidard.
DISCLOSURE: Dr. Bidard reported financial relationships with Archer, Lilly, Novartis Pharma SAS, Pfizer Pharmaceuticals Israel, Radius Health, AstraZeneca, Roche, Amgen, Chugai Pharma, and Menarini Silicon Biosystems.
REFERENCE
1. Bidard FC, Callens C, Dalenc F, et al: Prognostic impact of ESR1 mutations in ER+ HER2– MBC patients with prior treatment with first-line AI and palbociclib: An exploratory analysis of the PADA-1 trial. ASCO20 Virtual Scientific Program. Abstract 1010.



