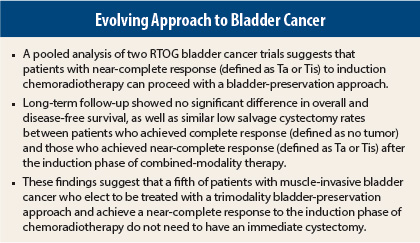
Organ preservation is a hallmark of progress in the world of cancer management. For patients with muscle-invasive bladder cancer, the bladder-sparing approach is a well-established alternative to radical cystectomy. Patients undergo cystoscopic evaluation between the induction and consolidation phases of chemoradiation, and patients with an incomplete response to the induction phase are promptly offered cystectomy. A retrospective pooled analysis of two multi-institutional trials found no difference in disease-specific, bladder-intact, and overall survival between patients with a complete response or near-complete response to induction chemoradiation.1
Pooled Analysis
“These results suggest that it is appropriate to recommend that patients with near-complete response to induction chemoradiation be continued on bladder-preserving therapy,” said lead author Timur Mitin, MD, PhD, of the Department of Radiation Medicine at the Oregon Health and Science University, Portland.
The study was based on a pooled analysis of two Radiation Therapy Oncology Group (RTOG) trials (9906 and 0233) to determine long-term outcomes among patients with muscle-invasive bladder cancer who achieve either complete or a near-complete response after induction chemoradiotherapy. Results were presented at the 2014 Genitourinary Cancers Symposium in San Francisco.
Bladder-conservation therapy has been around in Europe and North America for about 4 decades, but the current backbone of the trimodality bladder-preservation approach, used in the United States, includes maximal transurethral resection of bladder tumor (TURBT), followed by radiation with concurrent chemotherapy, Dr. Mitin explained. Patients undergo cystoscopic evaluation with biopsies after the first phase of chemoradiation induction. Patients with complete response go on to receive a consolidation phase of chemoradiotherapy. Otherwise patients undergo radical cystectomy, he said.
Relaxed Criteria
“Historically, complete response after cystoscopic evaluation has been defined as T0 (no tumor), but many physicians have been reluctant to offer radical cystectomy to patients with only a small amount of noninvasive tumor (Ta) or carcinoma in situ (Tis), following induction chemoradiation,” Dr. Mitin told the audience.
Both trials had relaxed criteria for requiring salvage cystectomy and allowed patients with Ta or Tis after the induction to continue with consolidation chemoradiation. RTOG 9906 was a single-arm trial of 80 patients who received paclitaxel/cisplatin plus twice-daily radiation following transurethral resection of bladder tumor. RTOG 0233 was a phase II trial that randomly assigned 97 patients post–transurethral resection of bladder tumor to twice-daily radiation with either paclitaxel/cisplatin or fluorouracil/cisplatin. The radiation dose and techniques were the same in the two trials.
The pooled analysis of outcomes included 119 eligible patients: 101 with complete response (85%) and 18 with near-complete response (Ta or Tis, 15%). Median age was 65 years among complete responders and 70 years among near-complete responders. The majority of patients had clinical stage T2 at diagnosis.
Major Findings
At a median follow-up of 5.9 years, 5-year survival was 72% among complete responders and 61% among near-complete responders, which was not statistically significant. Disease-free survival was also not statistically different between the two groups of patients.
Among 101 patients with complete response after induction, 13 developed invasive bladder recurrence (13%), eventually requiring salvage cystectomy. Among 18 patients with near-complete response, there was one invasive bladder recurrence (6%), and this patient required salvage
cystectomy.
“Although this is a small retrospective analysis, there is no apparent difference in bladder recurrence and salvage cystectomy rates between complete responders and near-complete responders as judged at the time of cystoscopic evaluation after the induction phase of bladder-preserving trimodality therapy,” Dr. Mitin emphasized. n
Disclosure: Dr. Mitin reported no potential conflicts of interest. For full disclosures of the study authors, visit abstracts.asco.org. ■
Reference
1. Mitin T, George A, Zietman AL, et al: Long-term outcomes among patients who achieve complete or near-complete responses after the induction phase of bladder-preserving combined modality therapy for muscle-invasive bladder cancer: A pooled analysis of RTOG 9906 and 0233. 2014 Genitourinary Cancers Symposium. Abstract 284. Presented January 31, 2014.