The availability of the tyrosine kinase inhibitor imatinib (Gleevec) has dramatically increased survival in chronic myeloid leukemia (CML). Nonadherence to therapy with imatinib and other tyrosine kinase inhibitors is associated with disease progression and treatment resistance. In a study reported in the Journal of Clinical Oncology, Stacie B. Dusetzina, PhD, University of North Carolina at Chapel Hill, and colleagues evaluated trends in imatinib expenditures from 2002 to 2011 and the association between copayment requirements for imatinib and tyrosine kinase inhibitor adherence.1 They found that patients with higher copayments are significantly more likely to be nonadherent to or discontinue tyrosine kinase inhibitor treatment.
Study Details
The study involved review of MarketScan health plan claims to identify patients aged 18 to 64 years with CML who started imatinib therapy between January 2002 and June 2011 and had insurance coverage for ≥ 3 months before and ≥ 6 months after treatment initiation (N = 1,541). The primary outcomes were tyrosine kinase inhibitor discontinuation and nonadherence. The primary independent variable was out-of-pocket cost for a 30-day supply of imatinib.
A propensity-score weighted sample was used to estimate risk of discontinuation and nonadherence for patients with higher (top quartile) vs lower copayments (bottom 3 quartiles). The propensity score was derived by modeling the probability of having higher vs lower copayments as a function of control variables including age, insurance type, region, and enrollee relationship to employee, all assessed in the month prior to starting therapy, as well as the Klabunde modification of the Charlson comorbidity score and number of medication classes used preceding treatment initiation, both assessed during the 3 months prior to the start of therapy.
Copayments
Copayment requirements were calculated based on coinsurance or copayments for the first fill for imatinib. Most patients paid copayments (88.5% of imatinib users) rather than coinsurance (6% of imatinib users). Costs varied substantially, with 6% of patients paying > $500 for a 30-day supply.
Over the study period, the mean copayment for a 30-day supply of imatinib was $108 and the median copayment was $30, with a range of $0 to $4,792. Although mean monthly copayments varied widely (from $0 to $4,792 for a 30-day supply), patients in the lowest 25th percentile were paying $17 and those in the upper 75th percentile were paying $53. Monthly copayments increased from an average of $55 in 2002 to $145 in 2010. Mean monthly total expenditure for imatinib increased from $2,798 in 2002 to $4,892 in 2011 ($2,846 to $4,954 for median expenditure).
Before propensity-score weighting, patients with relatively lower imatinib copayment requirements (lowest 3 quartiles, n =1,134) and those with higher copayment requirements (upper quartile, n = 407) were generally balanced for age (mean, 49 and 48 years), sex (44% and 46% female), relationship of patient to employee (66.5% and 69% employee), starting imatinib dose (≤ 400 mg in 89% in both), number of medications in the 3 months before start of treatment (mean, 5.5 and 5.3), and Charlson comorbidity score (0 in 94% and 95%).
Patients with higher copayment requirements were significantly less likely to live in the Northeast (13% vs 8%, P = .01 for trend) and significantly more likely to have a preferred provider organization health plan (57% vs 68%, P < .001 for trend). After propensity-score weighting, there were no significant differences between groups in any of these characteristics.
Discontinuation and Nonadherence
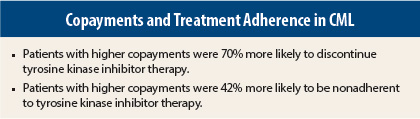
On adjusted analysis, 10% of patients with lower copayment requirements and 17% with higher requirements discontinued therapy during the first 180 days after treatment initiation, representing a 70% increase in risk of discontinuing tyrosine kinase inhibitors in those with higher copayments (adjusted risk ratio [RR] = 1.70, 95% confidence interval [CI] = 1.30–2.22). Similarly, patients with higher copayments were significantly more likely to be nonadherent with tyrosine kinase inhibitor therapy, defined as < 80% of days with drug available (21% vs 30%, adjusted RR = 1.42, 95% CI = 1.19–1.69).
Patients with lower copayments had a significantly greater number of days covered by medication supply (87% vs 82%, adjusted risk difference = −0.05, 95% CI = −0.07 to −0.02), but there was no difference between groups when patients who discontinued medication were excluded from analysis (93% vs 92%, adjusted risk difference = −0.01, P = .15).
Sensitivity Analyses
Sensitivity analyses excluding patients who were hospitalized after starting imatinib, excluding patients who paid drug deductibles, excluding patients who were enrolled for < 6 months without tyrosine kinase inhibitor use, defining adherence as < 85% and < 90% of days covered, and defining discontinuation as > 90 days of no tyrosine kinase inhibitor treatment all had results consistent with the primary analysis.
An additional sensitivity analysis assumed that the confounder of poor understanding of one’s disease was twice as common among patients in the higher copayment group vs the lower copayment group (approximately 20% vs 10%) and assumed that the confounding factor was associated with a twofold increase in risk of discontinuation or nonadherence.
Based on these assumptions, risk of discontinuation and risk of nonadherence in the high copayment group remained significant. It was estimated that lack of understanding would need to be three times more common in the higher copayment group and associated with a threefold increased risk of discontinuation or adherence for the risk associated with higher copayment to no longer be significant.
The investigators concluded, “Patients with higher copayments are more likely to discontinue or be nonadherent to [tyrosine kinase inhibitors]. Given the importance of these therapies for patients with CML, our data suggest a critical need to reduce patient costs for these therapies.” ■
Disclosure: The study authors reported no potential conflicts of interest.
Reference
1. Dusetzina SB, Winn AN, Abel GA, et al: Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol. December 23, 2013 (early release
online).