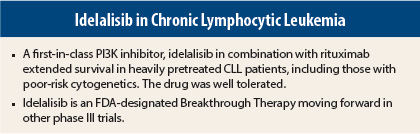
Idelalisib plus rituximab (Rituxan) improved progression-free survival, overall response rates, and overall survival compared with rituximab alone in heavily pretreated patients with relapsed chronic lymphocytic leukemia (CLL). Moreover, the combination provided effective, durable disease control in these patients, who were not suitable for cytotoxic chemotherapy.1
Highly Selective Oral Agent
“This study heralds the dawn of a new age, with the opportunity to treat CLL patients with refractory disease and to treat them much more safely,” stated Richard R. Furman, MD, Richard A. Stratton Associate Professor in Hematology and Oncology at Weill Cornell Medical College, New York. “Idelalisib represents an important addition to the armamentarium for patients living with this life-threatening disease.”
Idelalisib is a targeted, highly selective, orally administered inhibitor of the delta isoform of the PI3K enzyme, which is found exclusively in hematopoietic cells and is essential to survival of CLL cells. The drug inhibits cell proliferation and induces apoptosis of CLL cells. It also inhibits homing and retention of CLL cells in lymphoid tissues, reducing cell survival, Dr. Furman explained at a late-breaking abstract session during the 2013 American Society of Hematology (ASH) Annual Meeting in New Orleans. These properties of idelalisib explain the rapid and dramatic reduction in lymphadenopathy seen with this drug, before lymphocyte counts are reduced, he said.
Study 116
Study 116 was a randomized controlled, double-blind study conducted in the United States and Europe investigating the benefit of rituximab plus idelalisib compared with rituximab plus placebo. Eligible patients were considered unfit for chemotherapy, as defined by a Cumulative Illness Rating Scale (CIRS) score > 6, creatinine clearance < 60 mL/min, or myelosuppression secondary to prior chemotherapy.
A total of 220 patients were randomly assigned between the two arms. At baseline, both treatment arms were well balanced. The median number of prior therapies was three in each arm, 91% in the idelalisib arm and 88% in the placebo arm had received prior rituximab, and time since diagnosis was 7.8 and 8.6 years, respectively.
All patients received rituximab at 375 mg/m2, followed by 500 mg/m2 every 2 weeks for four doses, and then every 4 weeks for three doses, for a total of eight doses over 6 months. Idelalisib was administered at a dose of 150 mg twice daily. Patients continued on either idelalisib or placebo until disease progression, at which point they were given idelalisib at 150 mg twice daily in addition to their current therapy. Thus, patients initially on placebo received idelalisib at 150 mg plus placebo twice daily and patients initially on idelalisib at 150 mg received idelalisib at 300 mg twice daily.
The study was stopped early based on a prespecified interim analysis by an independent monitoring committee showing a highly statistically significant effect of idelalisib/rituximab on progression-free survival, the primary endpoint. Median progression-free survival was not reached in the idelalisib/rituximab arm vs 5.5 months in the rituximab/placebo arm (P < .0001), representing an 85% improved likelihood of progression-free survival with the novel agent. For all prespecified subgroups, progression-free survival favored idelalisib/rituximab over placebo/rituximab.
Overall survival also favored idelalisib/rituximab over rituximab/placebo (P = .018). A decrease in lymphadenopathy, based upon “nodal response” (which required a > 50% reduction), was seen in 93% of the idelalisib/rituximab arm vs 4% of the placebo/rituximab arm.
Adverse events were similar in both arms: 90.9% and 94.4%, respectively, experienced any adverse event; 56.4% and 47.7%, respectively, experienced grade 3 or higher adverse events. There were fewer deaths in the idelalisib/rituximab arm: 4 vs 12, respectively. Infusion-related reactions occurred in 17 patients (16%) in the idelalisib/rituximab arm vs 30 patients (28%) in the rituximab/placebo arm.
Eliminating Chemotherapy
Based on these findings, idelalisib was granted Breakthrough Therapy designation for CLL by the U.S. Food and Drug Administration.
“With drugs like idelalisib, we have a great opportunity to eliminate chemotherapy from the treatment paradigm. The focus has always been on eliminating chemotherapy for patients who are unfit and likely to suffer toxicities. My hope is that with these novel agents (tyrosine kinase inhibitors), even medically fit patients will be able to avoid chemotherapy and its toxicities, making long-term survival a reality,” Dr. Furman commented. ■
Disclosure: Dr. Furman has served as an advisor for Gilead Sciences.
Reference
1. Furman RR, et al: ASH Annual Meeting. Abstract LBA-6. Presented December 10, 2013.