Sentinel node status is “the most powerful predictor” of melanoma-specific survival in patients with thin melanoma, according to a presentation at the 2014 Society of Surgical Oncology (SSO) Cancer Symposium in Phoenix.1 As a result, sentinel lymph node biopsy should be considered in patients with melanoma less than 0.70 mm, concluded Genevieve Boland, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and colleagues. In addition, the presence of mitotic activity and/or Clark level IV/V was associated with an increased risk of positive sentinel lymph node status.
Dr. Boland’s research was one of two papers on the role of sentinel node biopsy in thin melanoma presented during an SSO Parallel Session on Melanoma. In the second, Mark Faries, MD, of the John Wayne Cancer Institute in Santa Monica, California, and colleagues compared outcomes among patients with thin melanoma who presented with sentinel node metastases and patients who developed clinical node recurrence.2
Predictors of Survival
“We know from various studies, including the MSLT I [Multicenter Selective Lymphadenectomy Trial I], that sentinel lymph node biopsy is one of the most powerful predictors of recurrence and survival in patients with intermediate-thickness and thick melanoma,” Dr. Boland said. “It has become the standard of care for patients with tumors > 1 mm.”3
However, a large proportion of people who present in the clinic do so with thin melanoma, and this cohort of patients was not included in the MSLT1 trial, she said. “So the role of sentinel lymph node biopsy in thin melanoma is not well defined,” she added.
Dr. Boland’s group examined clinicopathologic factors and sentinel lymph node status, along with melanoma-specific survival, in a contemporary clinical cohort (1999–2009). From a prospective database, they identified patients with clinically node-negative melanoma (≤ 1 mm) who also had wide excision and underwent sentinel node biopsy at MD Anderson Cancer Center.
The study cohort consisted of 867 patients whose thin melanomas had a median Breslow thickness of 0.70 mm. Among those patients, 3% experienced ulceration, 45% had mitosis of ≥ 1 mm2, and the sentinel lymph node rate was 5%.
The authors identified the most dominant predictors of a positive sentinel lymph node as increasing Breslow thickness > 0.7 mm (vs < 0.7 mm, odds ratio [OR] = 5.6, P < .0001) and increasing mitosis ≥ 1 mm2 (vs < 1 mm2, OR = 4.0, P = .0001). They also noted that Clark level IV/V (vs II/III, OR = 3.1, P = .0002) was another statistically significant factor.
“We chose to address these dominant factors a little more closely,” Dr. Boland said. “When we stratified the patient by a cutpoint of 0.7 mm … in the < 0.7-mm [group], there was a 2% incidence of positive sentinel lymph node vs 9% in the > 0.7-mm group. Among patients with the highest Breslow thickness, [there was] an increase in the incidence of positive sentinel lymph node rate to 12% when the mitotic rate was equal to or greater than 1 mm2.”
Melanoma-Specific Survival
With regard to melanoma-specific survival, at a median follow-up of 6.8 years, the 5-year melanoma-specific survival was 98.5%. The following factors were associated with poorer melanoma-specific survival:
- Breslow thickness: 0.7–1.0 mm (P = .0065)
- presence of mitosis (P = .0017)
- AJCC stage T1b (P = .0032)
- age > 60 years at diagnosis (P = .0083)
The 5-year melanoma-specific survival was 99% in patients with negative sentinel lymph nodes and 85% in those with positive nodes (P < .0001).
In a multivariate analysis, the two independent factors predictive of melanoma-specific survival were positive vs negative sentinel lymph node status (hazard ratio [HR] = 36.57, 95% confidence interval [CI] = 14.84–90.3, P < .0001) and age at diagnosis (HR = 1.07, 95% CI = 1.03–1.10, P < .0001). There were 20 melanoma-specific deaths in the cohort, Dr. Boland reported.
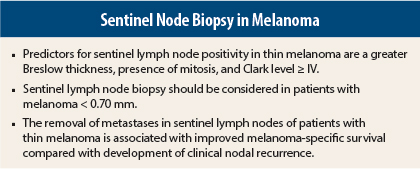
“The predictors that we found in our cohort of patients for sentinel lymph node positivity were a greater Breslow thickness, presence of mitosis, and Clark level greater than or equal to IV,” she said. “Stratifying patients according to this range, the sentinel lymph node–positive rate was 1% to 12%.”
The authors concluded that sentinel lymph node status is a dominant predictor of melanoma survival. “There are likely some subsets of patients for whom the risk of a positive sentinel lymph node may be sufficient to offer them a sentinel lymph node biopsy, and we may be able to use clinicopathologic factors to stratify out the appropriate patients,” Dr. Boland stated.
Selection Bias Issues
During the question-and-answer session, Dale Han, MD, of Yale University School of Medicine in New Haven, Connecticut, pointed out that “this is a very selective patient population. You show a 2% rate in your 0.7-mm population, but that’s probably even lower if you encompass all patients with 0.7 mm. Even when you substratify by mitotic rates, it’s still 4% at most.”
Dr. Boland replied that “this is not the definitive guideline. We’ve selected out high-risk patients from the baseline, so this is not the average patient who is going to walk into the clinic…. There may be questions of biology; if our surveillance is good, we may catch bad biology early.”
Daniel Coit, MD, of Memorial Sloan Kettering Cancer Center in New York, also brought up the issue of selection bias and suggested that the study authors were “making this way too complicated.”
He continued, “I think you have a much simpler question to answer: What’s the threshold for doing a sentinel lymph node biopsy in an otherwise healthy, 40-year-old person—I’m going to pick an average age—and should that threshold be the same in America as it is in Australia; should it be the same around the world?”
Dr. Boland’s coauthor Jeffrey Gershenwald, MD, also of MD Anderson, responded to Dr. Coit’s question. “On a global level, for young, healthy patients, many people have considered a threshold of 5% as a starting point for discussion. Clearly, for someone with comorbidities, older age, etc, a threshold of 10% or more might just barely scratch the surface for offering someone the procedure,” he said.
“There are lots of way we could do a lot more,” Dr. Gershenwald added. “This [current study] is one snapshot of one way to present data.”
Survival Advantage?
Dr. Faries and colleagues sought to answer the question, is there a survival advantage to early treatment of lymph node metastases for patients with thin melanomas? They conducted a retrospective comparison of patients who had nodal disease, identified either by sentinel lymph node metastases or clinical node recurrence.
They used data from two independent, prospectively maintained melanoma databases: one at John Wayne Cancer Institute (center 1) that tracked patients with positive sentinel lymph nodes from 1986 to 2010 and clinical node recurrence from 1971 to 2010, and one at the University of Pennsylvania in Philadelphia (center 2). The latter included sentinel lymph node–positive patients from 1996 to 2011 and a historic cohort with nodal recurrence from 1973 to 1989. From both centers, the authors looked at patient demographics, pathologic characteristics, and survival from primary melanoma diagnosis. They then compared survival between center 1 and center 2.
When compared with nodal recurrence patients, sentinel lymph node patients at center 1 were older, had more ulcerated tumors, elevated Clark level (P < .0001 for all) and a trend toward increased Breslow thickness. At center 2, sentinel lymph node patients had increased Clark level and Breslow thickness, increased mitosis, and increased overall T stage, but a lower frequency of ulcerations.
Multivariate Analysis
In a multivariate analysis, the following were all prognostic variables for decreased melanoma-specific survival:
- age > 50 (HR = 1.48, 95% CI = 1.15–1.89, P = .002)
- ulceration (HR = 1.86, 95% CI = 1.19–2.93, P = .007)
- truncal site (HR = 1.60, 95 CI = 1.17–2.20, P = .004)
- method of nodal disease discovery, ie, clinical nodal recurrence vs positive sentinel lymph node (HR = 3.34, 95% CI = 1.86–6.02, P < .001)
The 5-year survival rate for the sentinel lymph node–positive patients was 88% vs 72% for the nodal recurrence group. The 10-year survival was 84% vs 49%, respectively (P < .0001).
“The removal of metastases in sentinel lymph nodes of patients with thin melanoma is associated with improved melanoma-specific survival compared with development of clinical nodal recurrence,” Dr. Faries concluded. “This may reflect tumor biology, … patient selection, or potential therapeutic efficacy of sentinel lymph node biopsy in thin melanoma.”
Varied Reactions
The study results elicited very different responses from the SSO attendees. Mary Sue Brady, MD, of Memorial Sloan Kettering Cancer Center, said that she thought this analysis was an oversimplification. “I’ve never believed that people [for whom treatment fails] clinically are the same as people with microscopic disease,” she explained. “I think it’s much more complex than that.”
But Merrick Ross, MD, of MD Anderson Cancer Center, praised the study results. Addressing the issue of differences in patients, Dr. Ross stated, “maybe these are different patients; maybe they are different now because you’ve allowed them to have the metastasis grow in the lymph node for 5 years or 10 years, and they become different because the cells mutate.… Until we find a better way to identify these high-risk patients, this seems like a pretty good way.” He added, “In the absence of a prospective, randomized trial, which will never be done, … these data should not be dismissed.” ■
Disclosure: Dr. Boland reported no potential conflicts of interest. Dr. Faries has served as a consultant for Genentech and as an investigator/proctor for Delcath Systems.
References
1. Boland G, Caudle A, Warneke C, et al: Predictors of survival in contemporary era patients with thin melanoma who underwent sentinel node biopsy. 2014 SSO Cancer Symposium. Abstract 53. Presented March 14, 2014.
2. Faries MB, Karakousis GC, Bartlett E, et al: Improved survival in patients with thin melanoma after positive sentinel node versus clinical nodal recurrence. 2014 SSO Cancer Symposium. Abstract 54. Presented March 14, 2014.
3. Howard JH, Thompson JF, Mozzillo N, et al: Metastasectomy for distant metastatic melanoma: Analysis of data from the first Multicenter Selective Lymphadenectomy Trial (MSLT-I). Ann Surg Oncol 19:2547-2555, 2012.