The antibody-drug conjugate rovalpituzumab tesirine has shown strong clinical activity as second- and third-line treatment for small cell lung cancer in a phase I/Ib multicenter study,1 especially in the subset with high expression of the delta-like protein 3 (DLL3), which the drug targets. This finding also may point to the discovery of the first predictive biomarker associated with drug efficacy in this malignancy.
“[Rovalpituzumab tesirine] has manageable toxicity and demonstrates substantial single-agent antitumor activity and durability in patients with relapsed or refractory DLL3-positive small cell lung cancer (SCLC),” reported M. Catherine Pietanza, MD, of Memorial Sloan Kettering Cancer Center, New York. “The response rate is similar whether patients receive the drug second or third line.” Dr. Pietanza reported these emerging results from this first-in-human phase I trial of rovalpituzumab tesirine in recurrent SCLC at the 2015 European Cancer Congress.
Rovalpituzumab tesirine consists of a humanized monoclonal antibody, a dipeptide linker, and a pyrrolobenzodiazepine dimer toxin. It targets DLL3, a Notch ligand that is overexpressed in SCLC tumor–initiating cells but not in normal tissue. In DLL3-expressing patient-derived xenograft tumor models of SCLC, rovalpituzumab tesirine induced tumor regression and prolonged the time to progression, outperforming cisplatin/etoposide, investigators of a related preclinical publication noted.2
The 73 previously treated patients with progressive SCLC received rovalpituzumab tesirine as a single agent once every 3 or 6 weeks, in dose-escalating cohorts (0.05–0.8 mg/kg). Of these patients, 47% had primary refractory or resistant disease, and 45% had progressed after second-line therapy.
Dose-limiting thrombocytopenia and/or serosal effusions were observed at 0.8 and 0.4 mg/kg once every 3 weeks, respectively; therefore, these schedules were not pursued further. Pharmacokinetic data revealed a longer-than-expected half-life, encouraging a schedule of once every 6 weeks.
The phase Ib expansion cohorts received doses of 0.2 mg/kg once every 3 weeks or 0.3 mg/kg once every 6 weeks.
A DLL3 antibody was developed and utilized to assess antigen expression in archived tumor specimens. DLL3-high tumors were defined by immunohistochemistry membrane–associated H scores ≥ 180; within the study, 70% of the patients were DLL3-high, 11% had intermediate expression of DLL3, and 19% had low expression of DLL3.
Strong Activity in DLL3-Positive Patients
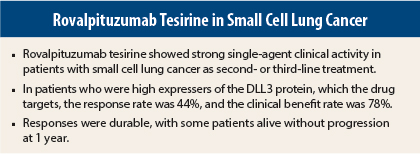
Among all evaluable patients in the dose-expansion cohorts, the objective response rate was 23%, and the clinical benefit rate was 68%. All responses were observed among DLL3-high patients; patients with stable disease had variable expression of DLL3.
Among the DLL3-high population, the response rate rose sharply to 44%, and 78% of patients achieved a clinical benefit. In this group, response rates were similar in the second- and third-line settings, and they exceeded 20%, even among patients who were refractory or resistant to their first line of treatment.
“Responses were durable,” Dr. Pietanza noted. At the 0.3 mg/kg schedule once every 6 weeks, there were seven responders, six of whom remained progression-free at a postresponse follow-up of a mean of 189 days or longer. The mean overall survival for this cohort was 236 days, with some patients surviving up to 1 year to date.
“For these reasons, 0.3 mg/kg once every 6 weeks is the recommended, phase II dose,” she added.
Unique Toxicities
“Safety was manageable,” reported Dr. Pietanza, although she described a “unique” toxicity profile for rovalpituzumab tesirine. The profile primarily includes serosal effusions (pleural, pericardial, peritoneal) and rash/photosensitivity, in addition to fatigue and thrombocytopenia.
“Effusions range from asymptomatic to those requiring drainage, and sometimes are recurrent,” she said. “Photosensitivity reactions occur in sun-exposed skin and may be most problematic during summer months.” ■
Disclosure: Dr. Pietanza reported no potential conflicts of interest.
References
1. Pietanza MC, Spigel D, Bauer TM, et al: Safety, activity, and response durability assessment of single agent rovalpituzumab tesirine, a delta-like protein 3 (DLL3)-targeted antibody drug conjugate, in small cell lung cancer. 2015 European Cancer Congress. Abstract 7LBA. Presented September 28, 2015.
2. Saunders LR, Bankovich AJ, Anderson WG, et al: A DLL3-targeted antibody-drug conjugate eradicated high-grade pulmonary neuroendocrine tumor-initiating cells in vivo. Sci Transl Med 7:302ra136, 2015.