While inhibitors of programmed cell death protein 1 (PD-1) or its ligand (PD-L1) are becoming established in melanoma, non–small cell lung cancer, and renal cell carcinoma, their efficacy is also being evaluated in numerous other tumor types, with promising results, according to studies presented at the 2015 European Cancer Congress in Vienna.
Urothelial Cancer
“Atezolizumab [formerly known as MPDL3280A] has the potential to change the standard of care in metastatic urothelial carcinoma,” according to Jonathan E. Rosenberg, MD, of Memorial Sloan Kettering Cancer Center, New York, who led the global phase II IMvigor 210 trial of the anti–PD-L1 drug in this malignancy.1 Patients with advanced bladder cancer have limited survival time, and no single agent has proven effective in extending lives, he noted.
IMvigor 210 included 311 patients, 78% of whom had received treatment for metastatic disease. The study enrolled “all comers,” but their PD-L1 expression was evaluated by immunohistochemistry, showing that two-thirds of patients had some degree of ligand expression.
“IMvigor 210 met its co–primary endpoints in [immune cell (IC) status] 2/3 (≥ 5% staining), IC1/2/3 (≥ 1%), and all-comer subgroups, demonstrating significant improvement over a historical 10% objective response rate,” Dr. Rosenberg announced.
“Durable responses were seen in a heavily pretreated population with metastatic urothelial carcinoma that progressed on platinum-based chemotherapy. Median duration of response was not reached in any [immune cell] or prognostic subgroup, including patients with liver metastases at baseline,” he said.
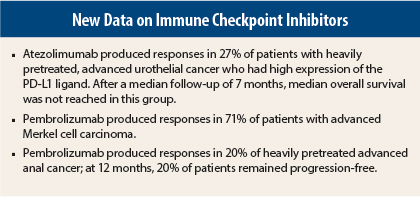
High PD-L1 status was associated with higher objective response rates. The highest, 27%, was seen in the IC2/3 subgroup (8% complete responses), 60% of whom had some decrease in target lesion size.
Responses were observed in 18% of the IC1/2/3 group (5% complete responses) and 15% in all comers (4% complete responses). Altogether, 43% of patients with tumor assessments had notable tumor shrinkage.
While the data remain immature at a median follow-up of 7 months, median overall survival was 7.9 months in all comers and was not reached in the IC2/3 subgroup. Median progression-free survival was 2.1 months in all groups.
“Atezolizumab was well tolerated, with no treatment-related deaths. The adverse event profile was consistent across IC2/3, IC1/2/3, and all-comer populations,” he added. Grade 3/4 toxicities were observed in 15% of patients, and 4% had a grade 3/4 immune-related event. No treatment-related renal toxicity was seen.
Ronald de Wit, MD, PhD, of Erasmus Medical Center, Rotterdam, the Netherlands, discussed the IMvigor 210 study. He noted that the initial results “show promising response rates and a survival benefit that seems promising vs historical controls.”
“We have to realize, though, that the high response rate to atezolizumab seems to be associated with [immunohistochemistry] positivity on immune cells. Unfortunately, high positivity accounts for only one-third of the patients,” he pointed out. “But we have encouraging data,” he said, not only with [atezolizumab] but also with pembrolizumab [Keytruda] and ramucirumab [Cyramza], in heavily pretreated patients.
At the 2015 European Cancer Congress, other investigators reported a 24% response rate to ramucirumab plus docetaxel and a median overall survival of 10.4 months.2 At the 2015 ASCO Annual Meeting, Plimack et al reported a 28% response rate and 13-month median overall survival with pembrolizumab.3
“These responses may be quite durable. There are promising overall survival data, and we have seen responses in patients with visceral metastases. So the data are promising, but we have to wait for the phase III results in an ongoing trial,” Dr. de Wit concluded.
Merkel Cell Carcinoma
Advanced Merkel cell carcinoma is typically a rapidly lethal tumor, associated with a median overall survival of less than 10 months. Anti–PD-1 agents may change the dire prognosis, based on the high response rates and durability of response observed in an open-label phase II study reported at the meeting by Paul Nghiem, MD, PhD, of the University of Washington in Seattle.4
The study included 24 patients who received pembrolizumab at 2 mg/kg for up to 2 years. Of the 14 patients with at least one post-treatment scan, 10 patients (71%) responded, 2 with complete responses. One patient had stable disease, and three had disease progression on treatment.
“Responses were rapid and appear more durable than we see with chemotherapy,” Dr. Nghiem said. “Pembrolizumab looks to be very favorable in terms of durability of response. With chemotherapy, at 90 days, half of our patients have progressed and gone off treatment.”
Many patients, he added, “have demonstrated profound shrinkage of tumor that has not rebounded.”
Anal Cancer
Pembrolizumab also demonstrated “promising, durable antitumor activity” in a heavily pretreated population of patients with PD-L1–positive squamous cell carcinoma of the anal canal, reported Patrick A. Ott, MD, PhD, of Dana-Farber Cancer Institute, Boston.5
In the phase Ib KEYNOTE-028 study, 25 pretreated patients received pembrolizumab. Responses to the anti–PD-1 agent were observed in 20% of patients (all partial), while 44% achieved stable disease. Median response duration has not been reached, Dr. Ott reported.
Median progression-free survival was 3.0 months. At 6 months, 31.6% were free of progression, and at 12 months, almost 20% still had not shown disease progression. ■
Disclosures: Dr. Rosenberg has received consulting fees from Bristol-Myers Squibb, Boehringer Ingelheim, Janssen, Oncogenex, Eli Lilly, Merck, and Agensys and owns stock in Merck. Dr. de Wit disclosed relationships with Merck and Eli Lilly. Dr. Nghiem reported no potential conflicts of interest. Dr. Ott is a consultant to Amgen and Bristol-Myers Squibb and has received research funding from ARMO Biosciences, Bristol-Myers Squibb, and Merck.
References
1. Rosenberg J, Petrylak D, Abidoye O, et al: Atezolizumab in patients (pts) with locally-advanced or metastatic urothelial carcinoma (mUC): Results from a pivotal multicenter phase II study (IMvigor 210). 2015 European Cancer Congress. Abstract 21LBA. Presented September 27, 2015.
2. Petrylak DP, Tagawa T, Kohl M, et al: Three-arm phase II randomized trial of docetaxel monotherapy or combined with ramucirumab or icrucumab in second-line locally advanced or metastatic urothelial carcinoma. 2015 European Cancer Congress. Abstract 2508. Presented September 27, 2015.
3. Plimack ER, Bellmunt J, Gupta S, et al: Pembrolizumab for advanced urothelial cancer: Updated results and biomarker analysis from KEYNOTE-012. 2015 ASCO Annual Meeting. Abstract 4502. Presented June 1, 2015.
4. Nghiem P, Bhatia S, Daud A, et al: Activity of PD-1 blockade with pembrolizumab as first systemic therapy in patients with advanced Merkel cell carcinoma. 2015 European Cancer Congress. Abstract 22LBA. Presented September 27, 2015.
5. Ott PA, Piha-Paul SA, Munster P, et al: Pembrolizumab (MK-3475) for PD-L1-positive squamous cell carcinoma (SCC) of the anal canal: Preliminary safety and efficacy results from KEYNOTE-028. 2015 European Cancer Congress. Abstract 500. Presented September 27, 2015.