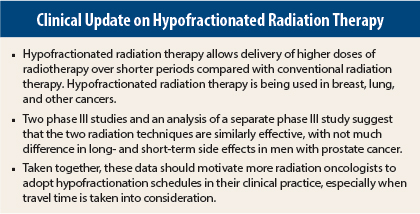
Several studies presented at the 2015 ASTRO Annual Meeting explored the use of hypofractionation (delivering higher doses of radiation in fewer fractions) in the treatment of patients with prostate cancer. These studies found comparable outcomes in terms of efficacy and adverse events. Although attractive from an economic point of view and from the patient convenience perspective, hypofractionation has not yet become the standard of care. The supportive evidence is mounting, however, and hypofractionation is gaining ground.
Intermediate- and High-Risk Patients
Five-year follow-up of the randomized phase III HYPRO trial showed that the rates of relapse-free survival for hypofractionated radiation therapy vs conventional fractionated radiotherapy were comparable in both men with intermediate- and high-risk prostate cancer (80% vs 77%, respectively).1 Acute toxicity was similar, with slightly higher gastrointestinal toxicity in the hypofractionated arm. Follow-up was too short to detect a survival benefit.
“Hypofractionated radiotherapy achieved a higher relapse-free survival rate compared with conventional fractionated radiotherapy, but the difference between the two arms was not statistically significantly different. The acute and late toxicities are comparable between the two schedules. At this point, we can say that hypofractionated radiotherapy is safe and of interest to be introduced in the clinic,” said lead author Luca Incrocci, MD, PhD, Professor of Genito-Urinary Radiotherapy at Erasmus MC Cancer Institute, Rotterdam, the Netherlands.
The HYPRO trial enrolled 820 patients with intermediate- or high-risk prostate cancer (stage T1b to T4) at 7 centers in the Netherlands between March 2007 and December 2010. Patients were randomized 1:1 to receive hypofractionated radiotherapy (19 fractions of 3.4 Gy in 6.5 weeks at 3 fractions per week) or conventional fractionated radiotherapy (39 fractions of 2 Gy in 8 weeks at 5 fractions per week). Baseline characteristics were similar between both arms of the study.
This study was designed as a noninferiority trial in intermediate- and high-risk patients. The median age of patients was 71 years, and about 66% were taking concomitant hormone therapy.
Acute gastrointestinal toxicity (grade 2 or higher) at 120 days was about 10% higher in the hypofractionated arm: 31.2% vs 42%, respectively. Acute genitourinary toxicity was 57.8% for the conventional arm vs 60.5% for hypofractionation, an absolute difference of 2.7%. The latter difference was not statistically significant.
Dr. Incrocci said that the late toxicity results will be published in the future, but he observed no significant differences in late genitourinary, gastrointestinal, and sexual function between the two arms.
Early-Stage Patients
RTOG 0415 was a randomized phase III noninferiority study that compared two fractionation schedules for intensity-modulated radiation therapy in low-risk early-stage prostate cancer2—a different patient population than in the HYPRO trial.
“Standard radiotherapy for prostate cancer takes 8–9 weeks, which can be a long-time commitment and somewhat daunting. Shorter treatments may be a better way to treat prostate cancer. Although shorter schedules have been assessed in single-institution studies, to date there have been limited definitive clinical trials,” said senior author Howard Sandler, MD, Professor and Chair of Radiation Oncology at Cedars-Sinai Medical Center in Los Angeles. W. Robert Lee, MD, MS, of Duke University, Chapel Hill, North Carolina, was the lead author of the RTOG 0415 study.
Men with early-stage, low-risk prostate cancer—defined as not palpable, prostate-specific antigen < 10 ng/mL, or Gleason score of 6 or lower—were randomized to receive standard radiation treatment over 8.2 weeks or hypofractionated treatment over 5.6 weeks.
In more than 300 men per arm followed for more than 5 years, 82% of the hypofractionated arm and 76% of the conventional arm were alive with no evidence of disease. This finding demonstrates noninferiority of the two schedules, Dr. Sandler stated.
Physician-reported toxicity showed no significant difference between the two arms in acute or late adverse events. A small absolute difference of 2.6% in gastrointestinal toxicity favored the conventional arm.
“These results suggest that this shorter regimen is a treatment regimen that physicians can be comfortable discussing and prescribing for their patients,” Dr. Sandler said.
He added that the data will have an impact on his clinical practice. “Standard treatment is standard fractionation, but for myself, I will change my practice based on these studies and offer hypofractionation to early-stage patients who progress on active surveillance as well as to selected patients in intermediate- and high-risk groups,” Dr. Sandler told listeners at a press conference at the 2015 ASTRO Annual Meeting.
Patient-Reported Outcomes
Long-term patient-reported outcomes showed no significant differences in short- and long-term quality of life in patients treated with hypofractionated radiation therapy vs conventional radiation therapy.3 These results were from a 5-year follow-up of a randomized phase III trial that found no difference in biochemical outcomes when hypofractionated radiation therapy was compared with conventional radiation therapy as primary treatment for 303 men with low- to high-risk prostate cancer.4
The radiation schedules compared in the trial follow: hypofractionated: 70 Gy in 26 fractions at 2.7 Gy per fraction; conventional radiation therapy: 76 Gy in 38 fractions at 2 Gy per fraction.
“Hypofractionated radiation therapy delivers higher doses per day with a shorter treatment time and reduced cost,” explained lead author Talha Shaikh, MD, Resident at Fox Chase Cancer Center, Philadelphia.
In the absence of long-term quality-of-life data to compare these two intensity-modulated radiation therapy techniques, patients were asked to complete three quality-of-life questionnaires: Expanded Prostate Cancer Index Composite (EPIC; 5 domains), International Prostate Symptom Score (IPSS; measure of urinary function), and the EuroQol (EQ-5D); they measure mobility, pain, and general health. There were no differences between the two arms of the trial on any of these measures at baseline.
No significant differences in long-term quality of life based on mean score change for EPIC bowel, sexual, hormonal, or urinary domains were reported. Patients in the hypofractionated arm exhibited a larger decrease in the EPIC urinary incontinence domain at 3 years vs the conformal radiotherapy arm, although this improved with further follow-up and was no longer significantly different after 5 years. On the IPSS, there was a trend for worse urinary function at 3 and 4 years in the hypofractionated arm, but this was improved with further follow-up.
Baseline function was the strongest predictor of outcomes, and Dr. Shaikh suggested that men with poor baseline urinary function should be counseled about the potential impact of hypofractionated radiation therapy on quality of life. ■
Disclosure: Drs. Incrocci and Shaikh reported no potential conflicts of interest. Dr. Sandler has spoken at a Varian User Group meeting and is on the medical advisory board of Eviti, part of NantHealth.
References
1. Incrocci L, Wortel RC, Aluwini A, et al: Hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year oncologic outcomes of the Dutch randomized phase 3 HYPRO trial. 2015 ASTRO Annual Meeting. Abstract LBA2. Presented October 18, 2015.
2. Lee WR, Dignam JJ, Amin M, et al: NRG Oncology RTOG 0415: A randomized phase III non-inferiority study comparing two fractionation schedules in patients with low-risk prostate cancer. 2015 ASTRO Annual Meeting. Abstract LBA 6. Presented October 19. 2015.
3. Shaikh T, Li T, Johnson ME, et al: Long-term patient reported outcomes from a phase 3 randomized prospective trial of conventional versus hypofractionated IMRT radiation therapy for localized prostate cancer. 2015 ASTRO Annual Meeting. Abstract 77. Presented October 19. 2015.
4. Pollack A, Walker G, Horwitz EM, et al: Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol 31:3860-3868, 2013.