 D. Neil Hayes, MD, MPH, of the University of North Carolina at Chapel Hill, described efforts to position the epidermal growth factor receptor (EGFR) inhibitor cetuximab (Erbitux) in head and neck cancer treatment.
D. Neil Hayes, MD, MPH, of the University of North Carolina at Chapel Hill, described efforts to position the epidermal growth factor receptor (EGFR) inhibitor cetuximab (Erbitux) in head and neck cancer treatment.
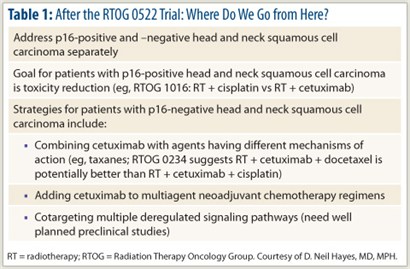
Surprisingly negative results came from the phase III Radiation Therapy Oncology Group (RTOG) 0522 trial (N = 940), which showed no benefit to adding cetuximab to the radiation/cisplatin platform for front-line therapy of advanced head and neck squamous cell carcinoma.1 At 2 years, progression-free survival was approximately 64% in both arms; overall survival was 79.7% with chemoradiation (P = .68) and 82.6% with the addition of cetuximab (P = .17). Rates of locoregional relapse and distant metastases were also similar.
Cetuximab increased grade 3/4 mucositis (43% vs 33%; P < .004), in-field skin toxicity (25% vs 15%; P < .001), and out-of-field skin reactions (19% vs 1%; P < .001), but toxicity beyond 90 days was similar between the arms.
 “RTOG 0522 was the study of the year in head and neck cancer. Unfortunately, it was flat-out negative,” Dr. Hayes noted.
“RTOG 0522 was the study of the year in head and neck cancer. Unfortunately, it was flat-out negative,” Dr. Hayes noted.
No differential effect emerged by p16 (HPV status). “While 70% of patients had oropharynx tumors (suggesting HPV positivity), tissue collection was lacking in half the patients. Our ability to make inferences with this amount of missing data is very limited,” Dr. Hayes said.
Even as a negative study, RTOG 0522 is practice-changing. “Many physicians have been treating with this regimen, assuming this study would be positive,” he said. “But we now have no data to support this.”
Cetuximab Equivalent to Cisplatin after Induction
The phase II TREMPLIN study (N = 153) evaluated sequential chemoradiotherapy in previously untreated, operable squamous cell carcinoma of the larynx/hypopharynx.2 Patients received induction chemotherapy with docetaxel, cisplatin, and fluorouracil; nonresponders underwent laryngectomy, whereas those with more than a 50% response were randomly assigned to radiotherapy plus either cisplatin or cetuximab.
All endpoints were similar between the arms. Larynx preservation rates at 3 months were 95% with cisplatin and 93% with cetuximab (P = .63). Preservation of larynx function at 18 months (or at death) was seen in 87% and 82%, respectively (P = .68). Overall survival was 92% and 89%, respectively (P = .44), and laryngoesophageal dysfunction-free survival was 79% vs 71% (P = .30). Acute toxicities compromising treatment and late toxicities were more common with cisplatin.
Dr. Hayes concluded, “The take-home message is that these two regimens are equivalent, and that cetuximab plus radiotherapy may be reasonable after induction.”
Laser Treatment Effective for Mucositis
In a phase III randomized trial of 94 patients, upfront use of low-level laser therapy helped prevent oral mucositis associated with chemoradiation.3 Grade 3/4 mucositis was observed in < 7% of the laser therapy group, compared with almost 50% of controls (who received “placebo” laser applications from the same machine but without light), for an 84% reduction (P < .001). Patients receiving active laser therapy also had less pain, narcotic use, and gastrostomia and better quality of life.
“Mucositis, especially grade 3 and 4, may limit treatment and compromise outcomes. While we need confirmatory data, the study shows we can intervene to improve mucositis.”
Future Directions
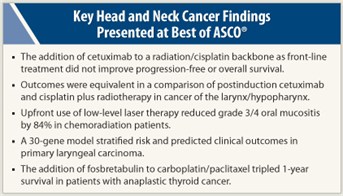 An international group developed a 30-gene expression profile that predicted clinical outcomes in primary laryngeal carcinoma.4 Median disease-free survival was 34 months in high-risk patients vs 80 months in low-risk patients (P = .01). Recurrences were four times greater among those in the high-risk group (P = .017).
An international group developed a 30-gene expression profile that predicted clinical outcomes in primary laryngeal carcinoma.4 Median disease-free survival was 34 months in high-risk patients vs 80 months in low-risk patients (P = .01). Recurrences were four times greater among those in the high-risk group (P = .017).
“This elegant study suggests subgroups of patients can be distinguished according to who will do well and who will do worse. For clinical usefulness, the issue is whether the difference between high- and low-risk groups will be sufficient to change therapy,” Dr. Hayes commented.
Finally, the novel vascular disrupting agent fosbretabulin (CA4P), combined with carboplatin and paclitaxel, tripled survival in the randomized phase II/III FACT trial (N = 80), from 9% at 1 year with chemotherapy alone to 26% (P = .065).5
“There is enthusiasm and excitement over this novel therapy for anaplastic thyroid cancer,” Dr. Hayes commented, urging oncologists to have patients enroll in the upcoming phase III trial. ■
Disclosure: Dr. Hayes reported receiving research funding from Lilly and honoraria from Bristol-Myers Squibb, Lilly, and sanofi-aventis.
SIDEBAR: Expert Q and A
References
1. Ang KK, Zhang QE, Rosenthal DI, et al: A randomized phase III trial (RTOG 0522) of concurrent accelerated radiation plus cisplatin with or without cetuximab for stage III-IV head and neck squamous cell carcinomas. 2011 ASCO Annual Meeting. Abstract 5500. Presented June 6, 2011.
2. Lefebvre J, Pointreau Y, Rolland F, et al: Results of the randomized phase II TREMPLIN study. 2011 ASCO Annual Meeting. Abstract 5501. Presented June 6, 2011.
3. Antunes HS, Herchenhorn D, Araujo CM, et al: Phase III trial of low-level laser therapy to prevent induced oral mucositis in head and neck cancer patients submitted to concurrent chemoradiation. 2011 ASCO Annual Meeting. Abstract LBA5524. Presented June 3, 2011.
4. Fountzilas E, Angouridakis N, Karasmanis I, et al: Prediction of clinical outcome in patients with primary laryngeal carcinoma using gene expression profiling. 2011 ASCO Annual Meeting. Abstract 5505. Presented June 6, 2011.
5. Sosa JA, Elisei R, Jarzab B, et al: Final survival analysis for the FACT trial. 2011 ASCO Annual Meeting. Abstract 5502. Presented June 6, 2011.

