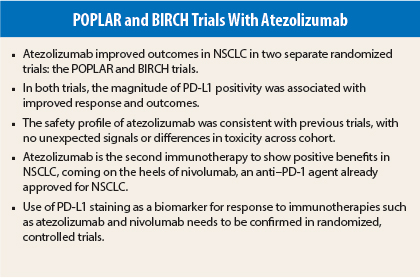
The anti–PD-L1 (programmed cell death-ligand 1) antibody atezolizumab (formerly known as MPDL3280A) achieved encouraging outcomes in patients with non–small lung cancer (NSCLC) in two different trials: POPLAR1 and BIRCH.2 PD-L1 has emerged as a predictive biomarker for atezolizumab response in both trials, which were presented at the 2015 European Cancer Congress and are part of a huge development program for this investigational immunotherapy.
According to ESMO spokesperson Martin Reck, MD, of the Hospital Grosshansdorf, Germany, “Atezolizumab is the second checkpoint inhibitor to show superior efficacy and better tolerability compared to second-line chemotherapy in patients with pretreated NSCLC. Therefore, it is to be expected that atezolizumab, like other PD-1 and PD-L1 antibodies, will substantially change treatment strategies of patients with refractory lung cancer.”
POPLAR Trial Details
“POPLAR demonstrated significant improvements in overall survival for unselected patients treated with atezolizumab vs docetaxel, reflecting a 27% improvement. Higher PD-L1 expression was associated with improved overall survival,” said lead author Johan Vansteenkiste, MD, PhD, of the University Hospitals Leuven, Belgium, who presented the trial results.
POPLAR was a randomized phase II trial that compared atezolizumab vs standard docetaxel in 287 patients with advanced NSCLC that progressed on prior platinum therapy. Patients were treated with atezolizumab until loss of clinical benefit and until disease progression in the docetaxel arm. The primary analysis presented by Dr. Vansteenkiste was on efficacy, safety, and predictive biomarkers.
Atezolizumab is an immunotherapy that inhibits PD-L1/PD-1 and PD-L1/B7 interactions and can restore antitumor T-cell activity and enhance T-cell priming. PD-L1 is thought to be a predictive biomarker and was measured with a proprietary SP142 assay sensitive and specific for PD-L1 expression on both tumor cells (TC) and immune cells (IC).
Patients in POPLAR were stratified according to their level of PD-L1 expression: TC3 and/or IC3 were considered high expressors; TC2/3 and/or IC2/3 were intermediate to high expressors. TC1/2/3 and/or IC1/2/3 were deemed “any expressors,” and TC0 and IC0 were deemed nonexpressors.
Baseline demographic and disease characteristics were well balanced between the two treatment arms. About two-thirds of patients had nonsquamous histology, and two-thirds received one prior platinum-containing regimen.
POPLAR Trial Results
Atezolizumab significantly improved overall survival from a median of 9.7 months with docetaxel to 12.6 months (P = .04), reflecting a 27% improvement favoring the anti–PD-L1 antibody. “At a minimum follow-up of 13 months, the emerging picture suggests that the separation of survival curves will be ongoing,” Dr. Vansteenkiste told listeners.
Median survival was even better in high expressors of PD-L1 (ie, TC3 or IC3). “We saw the benefit of increasing gradient according to expression of PD-L1,” he said, “with a 41% improvement in tumors with both TC3/IC3. In non–PD-L1 expressors, the survival curves are superimposed.”
“PD-L1 staining of tumor cells and immune cells is an independent predictor of survival improvement,” he noted.
The same phenomenon was observed for progression-free survival, with even a steeper gradient in improvement according to the intensity of PD-L1 expression.
Treatment-emergent grades 3-4 adverse events were 11% with atezolizumab vs 39% with docetaxel. The rate of grade 5 adverse events was 4% in both treatment arms. More patients in the docetaxel arm withdrew due to adverse events: 22% vs 8% for atezolizumab.
Alopecia, nausea, vomiting, and febrile neutropenia were more common with docetaxel, whereas immune-related events, such as dyspnea, pyrexia, arthralgia, musculoskeletal pain, and pneumonia, were more common with atezolizumab.
Dr. Vansteenkiste said the results of the phase III OAK trial of second-line atezolizumab patients with NSCLC are eagerly awaited. Multiple phase III trials that include atezolizumab in combination with other therapies are planned.
BIRCH Trial Details
POPLAR was not enriched for PD-L1 expression, whereas the BIRCH trial was a single-arm study of first-line or subsequent therapy that enrolled only PD-L1–positive patients with advanced or metastatic NSCLC (no brain metastasis allowed).
“The BIRCH trial found clinically meaningful results with atezolizumab monotherapy in PD-L1–selected patients with advanced NSCLC. The majority of responses are ongoing. Overall survival data are not mature. Six-month overall survival correlates with POPLAR results in second- and third-line therapy,” said lead author Benjamin Besse, MD, of Gustave Roussy, Paris. “The safety profile of atezolizumab is consistent with previous trials, with no unexpected signals or differences in toxicity across cohorts.”
“Higher PD-L1 expression correlates with higher responses and may identify NSCLC patients who are likely to benefit from atezolizumab therapy,” he added.
The study was stratified into three cohorts: Cohort 1 was treated with first-line atezolizumab until disease progression (n = 142); cohort 2 was treated with second-line atezolizumab after one prior platinum-containing therapy (n = 271); and cohort 3 was treated with third-line and higher atezolizumab (n = 254). These 667 patients were recruited from 100 sites in 19 countries.
The proprietary SP142 assay was used to prescreen more than 3,000 patients for PD-L1 positivity; 34% were found to be PD-L1 expressors, classified as TC2/3 and/or IC2/3. Of the overall eligible population, 46% were classified as high PD-L1 expressors (ie, TC3 or IC3).
Baseline clinical and pathologic characteristics were well balanced between the three treatment cohorts. Median age was 64 years, 59% were male, 72% had nonsquamous histology, 12% had EGFR mutations, and 33% had KRAS mutations.
BIRCH Trial Results
Overall response rates to atezolizumab were 17% in cohorts 2 and 3 and 19% in cohort 1. Overall response rates among high PD-L1 expressors were 27%, 24%, and 26%, in cohorts 1, 2, and 3, respectively. The majority of responses are ongoing.
Six-month overall survival was 82%, 76%, and 71% in cohorts 1, 2, and 3, respectively, and was higher when restricted to TC3 and IC3 patients (high expressors).
Six-month progression-free survival was 40%, 29%, and 31%, in cohorts 1, 2, and 3, respectively. Among TC3 or IC3 tumors, 6-month progression-free survival was 48%, 34%, and 39%, respectively, in cohorts 1, 2, and 3, respectively.
Of all patients, 11% had grades 3 or 4 treatment-related adverse events, which led to treatment discontinuation in 5%. Common adverse events included fatigue, diarrhea, nausea, pruritus, pyrexia, and decreased appetite.
Adverse events of special interest were reported in 26% of patients; the majority were grades 1 and 2. The most frequently occurring grade 3 and 4 adverse events of special interest were pneumonitis (1.5%, one fatal case), increased aspartate transaminase levels (0.8%), colitis (0.5%), hypothyroidism, and rash (0.3% for each). ■
Disclosure: The POPLAR and BIRCH trials were sponsored by Genentech. Dr. Reck has received honoraria for lectures and consultancy from Hoffmann-La Roche, Lilly, BMS, MSD, AstraZeneca, Boehringer Ingelheim, Novartis, and Pfizer. Drs. Vansteenkiste and Besse reported no potential conflicts of interest.
References
1. Vansteenkiste J, Fehrenbacher L, Spira AI, et al: Atezolizumab monotherapy vs docetaxel in 2L/3L non-small cell lung cancer: Primary analyses for efficacy, safety, and predictive biomarkers from a randomized phase II study (POPLAR). 2015 European Cancer Congress. Abstract 14LBA. Presented on September 27, 2015.
2. Besse B, Johnson M, Jänne PA, et al: Phase II singl-arm trial (BIRCH) of atezolizumab as first-line or subsequent therapy for locally advanced or metastatic PD-L1-selected non-small cell cancer. 2015 European Cancer Congress. Abstract 16LBA. Presented on September 27, 2015.