Several studies have addressed the risks and benefits of ovarian suppression during chemotherapy for breast cancer in women of childbearing age. A new meta-analysis of randomized trials found that it prevented premature ovarian failure and was associated with a higher number of pregnancies post chemotherapy without apparent negative consequence on prognosis. The study was presented at the 2015 European Cancer Congress and published to coincide with the presentation in Annals of Oncology.1,2
Attractive Option
“I hope our study will lead to ovarian suppression being deemed a valid option to be offered to patients for preservation of ovarian function and fertility,” stated Matteo Lambertini, MD, a coauthor of the study and a fellow in medical oncology at IRCCS AOU San Martino-IST, Genoa, Italy. Lucia Del Mastro, MD, of the same institution, is the corresponding author.
A diagnosis of breast cancer can be a major challenge, and for young women, the prospect of infertility may be devastating. “Pharmacologic protection of the ovaries with [luteinizing hormone–releasing hormone analog] during chemotherapy is an attractive option to preserve ovarian function and fertility. The agents are widely available, do not require any invasive procedure, and cause no delay in the initiation of anticancer therapy,” Dr. Lambertini said in a press release.
Women who need chemotherapy for breast cancer have the option of cryopreserving their eggs or embryos for future use prior to starting treatment. Dr. Lambertini said that ovarian suppression could be used in combination with these techniques “to increase the chance of fertility preservation as well as ovarian function after cancer therapies.”
Meta-analysis Details
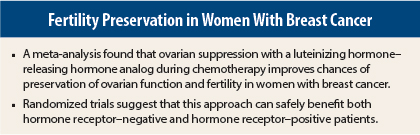
The meta-analysis included 12 randomized trials with a total of 1,231 breast cancer patients treated with chemotherapy with or without luteinizing hormone–releasing hormone analog. Ovarian suppression significantly reduced the number of cases of premature ovarian failure: 18.5% vs 33.5% for no ovarian suppression—a 64% reduction in the risk of developing this side effect (P < .001). However, these studies used different definitions of premature ovarian failure, and results were in a wide range.
The researchers then restricted the analysis to eight trials that included data on whether menstruation had restarted within 1 year after chemotherapy, which is the World Health Organization’s definition of menopause. In this restricted analysis, the results were in a similar range, showing a 45% reduction in the risk of developing chemotherapy-induced premature ovarian failure with luteinizing hormone–releasing hormone analog (P < .001). The subanalysis also revealed significantly lower 1-year rates of amenorrhea: 31% vs 42.9%, respectively (P < .001).
Of the original 12 studies, 5 included data on patients achieving pregnancies post treatment. Among 359 patients who received luteinizing hormone–releasing hormone analog during chemotherapy, 33 (9.2%) became pregnant vs 19 (5.5%) of 347 women who did not receive ovarian suppression during chemotherapy (P = .041). Pregnancy rates were similar across all five studies.
Three of the 12 studies looked at disease progression after chemotherapy with or without ovarian suppression and showed no difference in disease-free survival between women treated with luteinizing hormone–releasing hormone analog and those who were not: 19.5% vs 18.8%, respectively.
Current Guidelines
In a separate interview, Dr. Lambertini explained that current guidelines in this setting are not in agreement. ASCO guidelines from 2013 consider ovarian suppression “experimental” and state that the strategy should not be used outside of the context of a clinical trial. The POEMS study had positive results with ovarian suppression during chemotherapy in breast cancer patients, which led to its incorporation into the 2015 St. Gallen guidelines,3 and National Comprehensive Cancer Network guidelines4 also acknowledge the role of luteinizing hormone–releasing hormone analog in preventing chemotherapy-induced ovarian failure—but for both sets of guidelines, only in hormone receptor–negative breast cancer, as per study inclusion criteria of the POEMS trial.
The updated PROMISE-GIM6 study, including mostly hormone receptor–positive breast cancer patients, reported positive results for ovarian suppression at the 2014 Breast Cancer Symposium, also showing no detrimental effect on prognosis for concurrent administration of luteinizing hormone–releasing hormone analog and chemotherapy.5 Final results have been submitted for publication.
Dr. Lambertini noted that his meta-analysis included both the POEMS and PROMISE-GIM6 data. “Ovarian suppression could be useful and safe not only in hormone receptor–negative breast cancer, but also in those with hormone receptor–positive tumors, who account for two-thirds of new cases of breast cancer in young women,” he said. “Some guidelines favor this approach and others are hesitating to recommend it. To date, the role of this approach in fertility preservation remains controversial.” ■
Disclosure: Dr. Lambertini reported no potential conflicts of interest.
References
1. Lambertini M, Ceppi M, Poggio F, et al: Ovarian suppression with luteinizing hormone-releasing hormone agonists during chemotherapy as a strategy to preserve ovarian function and fertility in breast cancer patients. 2015 European Cancer Congress. Abstract 1957. Presented September 28, 2015.
2. Lambertini M, Ceppi M, Poggio F, et al: Ovarian suppression with luteinizing hormone-releasing hormone agonists during chemotherapy as a strategy to preserve ovarian function and fertility in breast cancer patients. Ann Oncol. September 7, 2015 (early release online).
3. Moore HC, Unger JM, Albain KS: Ovarian protection during adjuvant chemotherapy. N Engl J Med 372:2269-2270, 2015.
4. National Comprehensive Cancer Network: NCCN Guidelines Version 3.2015—Invasive Breast Cancer: Fertility and Birth Control. Available at http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed October 6, 2015.
5. Lambertini M, Boni L, Michelotti A, et al: Long-term outcome results of the phase III PROMISE-GIM6 study evaluating the role of LHRH analog during chemotherapy as a strategy to reduce ovarian failure in early breast cancer patients. 2014 Breast Cancer Symposium. Abstract 105. Presented September 4, 2014.