In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
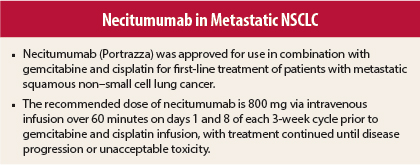
On November 24, 2015, necitumumab (Portrazza) was approved for use in combination with gemcitabine and cisplatin for first-line treatment of patients with metastatic squamous non–small cell lung cancer (NSCLC).1,2 Necitumumab is not indicated for treatment of nonsquamous NSCLC.
Supporting Efficacy Data
Approval was based on improvement in overall survival in an open-label phase III trial in which 1,093 patients were randomly assigned to receive necitumumab at 800 mg via intravenous infusion on days 1 and 8, gemcitabine at 1,250 mg/m2 on days 1 and 8, and cisplatin at 75 mg/m2 on day 1 of each 3-week cycle (n = 545) or gemcitabine/cisplatin alone (n = 548) until progression or unacceptable toxicity.2,3 Patients had a median age of 62 years, 83% were male, 84% were white, 92% were smokers, performance status was 0 or 1 for 91%, and 90% had metastatic disease in at least two sites.
Median overall survival, the primary endpoint, was 11.5 months (95% confidence interval [CI] = 10.4–12.6 months) in the necitumumab group vs 9.9 months (95% CI = 8.9–11.1 months) in the control group (hazard ratio [HR] = 0.84, P = .01). Median progression-free survival was 5.7 vs 5.5 months (HR = 0.85, P = .02). The objective response rate was 31% vs 29% (P = .40).
A lack of efficacy of necitumumab combined with pemetrexed (Alimta)/cisplatin vs pemetrexed/cisplatin alone in metastatic nonsquamous NSCLC was shown in a phase III trial that was closed prematurely after enrollment of 633 patients due to an increased incidence of death due to any cause and thromboembolic events in the necitumumab group.4 No improvement in overall survival (HR = 1.01, P = .96), progression-free survival (HR = 0.96, 95% CI = 0.8–1.16), or response rate (31% vs 32%) was observed with the addition of necitumumab in this setting.
How It Works
Necitumumab is a recombinant human IgG1 monoclonal antibody that binds to epidermal growth factor receptor (EGFR) and blocks the binding of EGFR to its ligands. Expression and activation of EGFR have been correlated with malignant progression, induction of angiogenesis, and inhibition of apoptosis.
Necitumumab binding induces EGFR internalization and degradation in vitro, as well as resulting in antibody-dependent cellular cytotoxicity in EGFR-expressing cells. In studies in mouse xenografts, including NSCLC, the addition of necitumumab to gemcitabine/cisplatin resulted in increased antitumor activity.
How It Is Used
The recommended dose of necitumumab is 800 mg via intravenous infusion over 60 minutes on days 1 and 8 of each 3-week cycle prior to gemcitabine and cisplatin infusion, with treatment continued until disease progression or unacceptable toxicity.
For grade 1 infusion-related reaction, the infusion rate should be reduced by 50%. For grade 2 infusion-related reaction, the infusion should be stopped until signs and symptoms have resolved to grade 0 or 1, with necitumumab resumed at a 50% reduced rate for all subsequent infusions. Treatment should be permanently discontinued for grade 3 or 4 infusion-related reaction.
Patients who have experienced a previous grade 1 or 2 infusion-related reaction should receive premedication with diphenhydramine hydrochloride (or equivalent) prior to all subsequent infusions. Those who have a second grade 1 or 2 infusion-related reaction should receive premedication for all subsequent infusions with diphenhydramine hydrochloride (or equivalent), acetaminophen (or equivalent), and dexamethasone (or equivalent).
Necitumumab should be withheld for grade 3 rash or acneiform rash until symptoms resolve to grade ≤ 2 and then resumed at a reduced dose of 400 mg for at least one treatment cycle. If symptoms do not worsen, the dose may be increased to 600 mg and 800 mg in subsequent cycles. Treatment should be permanently discontinued for grade 3 rash or acneiform rash that does not resolve to grade ≤ 2 within 6 weeks, reactions that worsen or become intolerable at a dose of 400 mg, grade 3 skin induration/fibrosis, and grade 4 dermatologic toxicity. Patients should be advised to limit sun exposure.
Treatment should be withheld for grade 3 or 4 electrolyte abnormalities. Subsequent cycles may be given once electrolyte abnormalities have improved to grade ≤ 2. Electrolytes should be replenished as necessary. Treatment should be discontinued for severe venous or arterial thromboembolic events.
Safety Profile
In the phase III trial supporting efficacy, the most common adverse events of any grade occurring at a frequency ≥ 2% higher in the necitumumab vs control group were rash (44% vs 6%), vomiting (29% vs 25%), and diarrhea (16% vs 11%). The most common grade 3 or 4 adverse events occurring at a ≥ 2% higher rate in the necitumumab group were venous thromboembolic events (5%, including pulmonary embolism, vs 3%), rash (4% vs 0.2%), and vomiting (3% vs 0.9%). Death attributed to cardiovascular events or sudden death was reported in 3% of the necitumumab group.
Hypomagnesemia of any grade occurred in 83% vs 70% of patients. Grade 3 or 4 electrolyte abnormalities included hypomagnesemia in 20% vs 7%, hypophosphatemia in 8% vs 6%, hypocalcemia in 6% vs 2% (albumin-corrected in 4% vs 2%), and hypokalemia in 5% vs 3%.
Necitumumab carries boxed warnings for cardiopulmonary arrest, sudden death, hypomagnesemia, and other electrolyte abnormalities when used in combination with gemcitabine/cisplatin. Serum electrolytes must be closely monitored during treatment, including monitoring for hypomagnesemia, hypocalcemia, and hypokalemia prior to each dose of necitumumab and for ≥ 8 weeks following treatment completion. Aggressive electrolyte replacement should be performed when warranted during and after treatment.
Necitumumab also carries warnings/precautions for cardiopulmonary arrest, hypomagnesemia and other electrolyte abnormalities, venous and arterial thromboembolic events, dermatologic toxicities, infusion-related reactions, increased toxicity and mortality if used in nonsquamous NSCLC, and embryofetal toxicity. Patients should not breastfeed during necitumumab treatment. ■
References
1. U.S. Food and Drug Administration: Necitumumab. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm474278.htm. Accessed December 14, 2015.
2. Portrazza (necitumumab) injection for intravenous use prescribing information, Eli Lilly and Company, November 2015. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2015/125547s000lbl.pdf. Accessed December 14, 2015.
3. Thatcher N, Hirsch FR, Luft AV, et al: Necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin alone as first-line therapy in patients with stage IV squamous non-small-cell lung cancer (SQUIRE): An open-label, randomised, controlled phase 3 trial. Lancet Oncol 16:763-774, 2015.
4. Paz-Ares L, Mezger J, Ciuleanu TE, et al: Necitumumab plus pemetrexed and cisplatin as first-line therapy in patients with stage IV non-squamous non-small-cell lung cancer (INSPIRE): An open-label, randomised, controlled phase 3 study. Lancet Oncol 16:328-337, 2015.