There are few treatment options for breast cancer patients with progressive disease after two or more HER2-directed regimens for recurrent or metastatic disease. In the open-label phase III TH3RESA trial reported in The Lancet Oncology by Ian E. Krop, MD, PhD, of the Dana-Farber Cancer Institute, Boston, and colleagues, ado-trastuzumab emtansine (Kadcyla) significantly prolonged progression-free survival compared with physician’s choice of therapy in patients with progressive HER2-positive advanced breast cancer who had received two or more HER2-directed regimens in the advanced setting, including trastuzumab (Herceptin) and lapatinib (Tykerb), and previous taxane therapy in any setting.1 Interim analysis showed an overall survival benefit of ado-trastuzumab emtansine that did not meet the stopping boundary.
Ado-trastuzumab emtansine is an antibody-drug conjugate consisting of the cytotoxic agent DM1 linked to trastuzumab. It was recently approved for single-agent use in patients with HER2-positive metastatic breast cancer who had previous treatment with trastuzumab and a concurrent or sequential taxane in any setting on the basis of findings in the phase III EMILIA trial.2 In this trial, ado-trastuzumab emtansine was associated with significant improvements in progression-free and overall survival and less severe toxicity compared with lapatinib plus capecitabine.
Study Details
In the TH3RESA trial, 602 adult patients from 22 countries in Europe, North America, South America, and Asia-Pacific with left-ventricular ejection fraction ≥ 50% and Eastern Cooperative Oncology Group (ECOG) performance status 0 to 2 were randomly assigned 2:1 between September 2011 and November 2012 to receive ado-trastuzumab emtansine at 3.6 mg/kg intravenously every 21 days (n = 404) or physician’s choice of treatment (n = 198).
Patients were stratified according to region (United States vs western Europe vs other), number of previous regimens (2–3 vs > 3), (excluding single-agent hormonal therapy) for the treatment of advanced disease and presence of visceral disease (any vs none). The coprimary endpoints were investigator-assessed progression-free and overall survival in the intention-to-treat population. The current report provides the final progression-free survival analysis and the first interim overall survival analysis.
The ado-trastuzumab emtansine and physician’s choice groups were generally balanced for age (median, 53 and 54 years), region (eg, Western Europe for 42% and 43%, United States for 25% and 24%), race (80% and 81% white, 14% and 12% Asian), ECOG performance status (0 in 45% and 41%, 1 in 50% and 51%, 2 in 5% and 8%), hormone receptor status (estrogen receptor– or progesterone receptor–positive in 51% and 52%, estrogen receptor– and progesterone receptor–negative in 46% and 43%), disease extent (metastatic in 97% and 94%), measurable disease (85% and 82%), median number of previous regimens for advanced disease (4 in both, including ≤ 3 in 33% and 39%, 4–5 in 37% and 33%, > 5 in 30% and 28%), median duration of exposure to trastuzumab (24 months in both) and lapatinib (8 months in both), and previously treated asymptomatic brain metastases (10% and 14%)
In the physician’s choice group, treatment consisted of combinations with a HER2-directed agent in 83%, including trastuzumab plus chemotherapy in 68% and trastuzumab plus lapatinib in 10%, and single-agent chemotherapy in 17%; chemotherapy use with or without HER2-directed therapy included vinorelbine in 32%, gemcitabine in 16%, eribulin (Halaven) in 9%, and paclitaxel in 9%.
Improved Progression-Free Survival
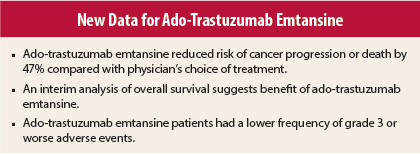
At the time of data cutoff (February 11, 2013), 44 patients assigned to physician’s choice had crossed over to ado-trastuzumab emtansine. After a median follow-up of 7.2 months in the ado-trastuzumab emtansine group and 6.5 months in the physician’s choice group, median progression-free survival was 6.2 months vs 3.3 months (stratified hazard ratio [HR] = 0.528, P < .0001). Median progression-free survival was also significantly improved with ado-trastuzumab emtansine compared with the subgroups of physician’s choice patients who received trastuzumab (6.2 vs 3.2 months, stratified HR = 0.558, P < .0001) or did not receive trastuzumab (6.2 vs 3.4 months, stratified HR = 0.428, P < .0001) as part of their regimen.
The progression-free survival benefit with ado-trastuzumab emtansine was consistent across subgroups, including significant hazard ratios according to age (0.55 for < 65, 0.42 for 65–74, and 0.14 for ≥ 75 years), hormone receptor status (0.56 for estrogen receptor– or progesterone receptor–positive, 0.51 for estrogen receptor– and progesterone receptor–negative), disease involvement (0.56 for visceral and 0.41 for nonvisceral involvement), number of previous regimens for advanced disease (0.48 for ≤ 3, 0.55 for >3), and previously treated asymptomatic brain metastases (0.47 for yes, 0.53 for no). The progression-free survival benefit was significant in the western Europe and other region subgroups but not in the U.S. subgroup (HR = 0.71, 95% confidence interval = 0.44-1.14).
At the time of the first interim overall survival analysis, death had occurred in 15% of the ado-trastuzumab emtansine group and in 22% of the physician’s choice group. Ado-trastuzumab emtansine was associated with reduced risk of death (stratified HR = 0.552, P = .0034); however, the result was not statistically significant, because it did not cross the prespecified O’Brien-Fleming stopping boundary of HR = 0.370 (which would have required a P value < .0000016).
Adverse Events
The most common adverse events of any grade in the ado-trastuzumab emtansine group were fatigue (27% vs 25% in the physician’s choice group), asthenia (16% vs 16%), and thrombocytopenia (15% vs 3%). Adverse events of grade 3 or higher occurred in 32% of the ado-trastuzumab emtansine group vs 43% in the physician’s choice group; neutropenia (2% vs 16%), diarrhea (< 1% vs 4%), and febrile neutropenia (< 1% vs 4%) were more common in the physician’s choice group and thrombocytopenia (5% vs 2%) was more common in the ado-trastuzumab emtansine group.
Serious adverse events occurred in 18% vs 21% of patients. No patients had a decrease in left-ventricular ejection fraction to < 40% in either group, and 1% of each group had a ≥ 15% absolute decrease in left-ventricular ejection fraction to < 50%. Grade 3 or higher hemorrhage of any type occurred in 9 (2%) ado-trastuzumab emtansine patients and in 1 (< 1%) physician’s choice patient. Adverse events led to dose reduction in 9% vs 20% of patients and to discontinuation of treatment in 7% vs 11%.
Death occurred in 5 (1%) patients in the ado-trastuzumab emtansine group and in 3 (2%) in the physician’s choice group. Three deaths in the ado-trastuzumab emtansine group (due to hepatic encephalopathy, subarachnoid hemorrhage, and pneumonitis) and one in the physician’s choice group (due to noncardiogenic pulmonary edema) were considered related to study treatment.
The investigators noted:
Together with EMILIA, findings from TH3RESA substantiate the potential of antibody–drug conjugates to achieve a more favourable benefit-to-risk profile than that seen with traditional combinations of chemotherapy and targeted agents in epithelial cancers. Data from these two large phase 3 studies suggest that trastuzumab emtansine is effective across the natural history of HER2-positive advanced breast cancer, spanning from disease with previous exposure only to adjuvant treatment, to progressive heavily pretreated disease after regimens incorporating trastuzumab and lapatinib.
They concluded, “Trastuzumab emtansine should be considered as a new standard for patients with HER2-positive advanced breast cancer who have previously received trastuzumab and lapatinib.” ■
Disclosure: The study was funded by Genentech. For complete disclosures of the study authors, visit www.thelancet.com.
References
1. Krop IE, Kim SB, González-Martín A, et al: Trastuzumab emtansine versus treatment of physician’s choice for pretreated HER2-positive advanced breast cancer (TH3RESA): A randomised, open-label, phase 3 trial. Lancet Oncol. May 1, 2014 (early release online).
2. Verma S, Miles D, Gianni L, et al: Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med 367:1783-1791, 2012.