As many as half of all patients with metastatic HER2-positive breast cancer develop brain metastases over time. The American Society of Clinical Oncology recently released a clinical practice guideline on disease management for patients with advanced HER2-positive breast cancer and brain metastases, published in the Journal of Clinical Oncology.1 A companion ASCO clinical practice guideline on systemic therapy for patients with advanced HER2-positive breast cancer has also been published in the Journal of Clinical Oncology (see coverage in the June 25 issue of The ASCO Post).2
The guideline recommendations were developed using evidence from observational studies and clinical experience. A literature search for evidence on brain metastases was conducted, but no publications met the inclusion criteria. On review of the available evidence, the ASCO expert panel concluded that the majority of the evidence was insufficient to inform evidence-based recommendations for a traditional ASCO clinical practice guideline.
Thus, the recommendations were developed by a multidisciplinary group of experts and reviewed by a consensus ratings panel including radiation oncologists, neurosurgeons, members of the ASCO Breast Cancer Guidelines Advisory Group, and others using a formal consensus process based on the best available evidence and clinical experience.
The ASCO expert panel was co-chaired by Sharon H. Giordano, MD, of The University of Texas MD Anderson Cancer Center, Houston, and Eric P. Winer, MD, of Dana-Farber Cancer Institute, Boston.
Guideline Questions
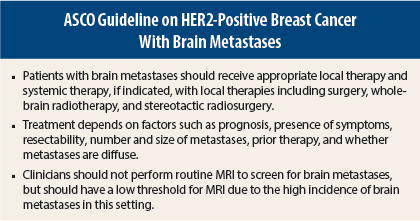
The overarching question addressed by the clinical practice guideline is: “What is the appropriate course of treatment for patients with HER2-positive advanced breast cancer and brain metastases?” The guideline recommendations are summarized below, according to four associated questions. A recommendation strength of weak was assigned to recommendations unless otherwise indicated; this rating indicates that there is some confidence that the recommendation offers the best current guidance for practice.
Recommendations
Does the approach to local therapy of brain metastases differ in patients with HER2-positive breast cancer?
Single Brain Metastasis, Favorable Prognosis
- Patients with favorable prognosis and a single brain metastasis should be evaluated by an experienced neurosurgeon for the option of surgical resection, particularly if the metastasis is > 3 to 4 cm or if there is evidence of symptomatic mass effect. (Evidence quality = intermediate, recommendation strength = strong.)
- Patients with favorable prognosis and a single brain metastasis < 3 to 4 cm without symptomatic mass effect may be offered either stereotactic radiosurgery or surgical resection, depending on the location and surgical accessibility of the tumor, need for tissue diagnosis, and other considerations, such as medical risk factors for surgery and patient preference. (Evidence quality = intermediate). If such patients choose to undergo stereotactic radiosurgery, clinicians may discuss the options of adding whole-brain radiotherapy to stereotactic radiosurgery. (Evidence quality = intermediate.)
- For most patients who undergo surgical resection, clinicians should recommend postoperative radiotherapy to the resection bed to reduce the risk of local recurrence. (Evidence quality = intermediate.)
- For patients with favorable prognosis and a single brain metastasis > 3 to 4 cm that is deemed unresectable and unsuitable for stereotactic radiosurgery, clinicians may discuss the options of whole-brain radiotherapy or fractionated stereotactic radiotherapy. (Evidence quality = low.)
- After treatment, serial imaging every 2 to 4 months may be used to monitor for local and distant brain failure. (Evidence quality = low.)
Limited Metastases, Favorable Prognosis
- In patients with favorable prognosis and multiple but limited metastases (2–4), treatment options depend on the size, resectability, and mass effect of the lesions.
- For patients with limited metastases suitable for stereotactic radiosurgery, clinicians may discuss stereotactic radiosurgery with or without whole-brain radiotherapy. (Evidence quality = intermediate.)
- For patients with a large (> 3 to 4 cm) lesion associated with symptomatic mass effect, clinicians may discuss surgical resection of the larger lesion. Remaining lesions may be treated with stereotactic radiosurgery with or without whole-brain radiotherapy. (Evidence quality = intermediate.)
- For patients with lesions that are unresectable and unsuitable for stereotactic radiosurgery, clinicians may recommend whole-brain radiotherapy and may discuss stereotactic radiosurgery after whole-brain radiotherapy. (Evidence quality = low.)
Diffuse Disease/Extensive Metastases
- For patients with symptomatic leptomeningeal brain metastases, clinicians may recommend whole-brain radiotherapy. (Evidence quality = low, recommendation strength = moderate.)
- For patients with more favorable prognosis and many diffuse brain metastases (≥ 5), clinicians may recommend whole-brain radiotherapy. (Evidence quality = low.)
Poor Prognosis
- For patients with poor prognosis, clinicians should discuss the options of best supportive care and/or palliative care, which may or may not include radiation therapy. (Evidence quality = low.)
- Patients with symptomatic brain metastases and poor prognosis may be offered whole-brain radiotherapy if there is a reasonable expectation of symptomatic improvement that outweighs acute and subacute treatment-related toxicities. (Evidence quality = low.)
Progressive Intracranial Metastases Despite Initial Therapy
- For patients with progressive intracranial metastases, treatment options depend on prior therapies, burden of disease, performance status, and overall prognosis.
Brain Recurrence and Irradiation, Limited Recurrence
- For patients with favorable prognosis and limited recurrence after treatment with whole-brain radiotherapy, clinicians may discuss stereotactic radiosurgery, a trial of systemic therapy, or enrollment onto a clinical trial. For those with favorable prognosis and limited recurrence after treatment with stereotactic radiosurgery, clinicians may discuss repeat stereotactic radiosurgery, surgery, whole-brain radiotherapy, a trial of systemic therapy, or enrollment onto a clinical trial. (Evidence quality = low, recommendation strength = moderate.)
Diffuse Recurrence
- For patients with diffuse recurrence after whole-brain radiotherapy, clinicians may discuss palliative options such as repeat reduced-dose whole-brain radiotherapy, a trial of systemic therapy, enrollment onto a clinical trial, or best supportive care. (Evidence quality = low.)
- For patients with diffuse recurrence after stereotactic radiosurgery, clinicians may discuss palliative options such as whole-brain radiotherapy, a trial of systemic therapy, enrollment onto a clinical trial, or best supportive care. (Evidence quality = low, recommendation strength = moderate.)
How should systemic therapy be managed in patients with HER2-positive brain metastases (including management of systemic therapy when the brain is the only site of progression vs when progression occurs in both the brain and elsewhere)?
- Systemic therapy should not be switched in patients who received a standard surgical- or radiotherapy-based approach, are receiving anti-HER2-based therapy, and do not have progressive systemic disease at the time of diagnosis. (Evidence quality = low, recommendation strength = moderate.)
- For patients receiving a standard surgical- and/or radiotherapy-based approach whose systemic disease is progressive at the time of brain metastasis diagnosis, clinicians should offer HER2-targeted therapy according to the algorithms for treatment of HER2-positive metastatic breast cancer. (Evidence quality = intermediate, recommendation strength = moderate.)
Is there a role for systemic therapy specifically to treat brain metastases in HER2-positive breast cancer?
- For patients with asymptomatic, low-volume brain metastases who have not received radiation therapy, clinicians may discuss upfront therapy with lapatinib (Tykerb) and capecitabine as an option. Patients should be informed that radiation therapy is still the primary option in this setting. (Evidence quality = low.)
- For patients developing intracranial disease progression after whole-brain radiotherapy or stereotactic radiosurgery (including those who are not candidates for reirradiation), clinicians may discuss systemic therapy as an alternative, using a regimen with some evidence of activity in CNS disease. (Evidence quality = low.)
Should patients with HER2-positive breast cancer be screened for development of brain metastases?
- Patients with no known history or symptoms of brain metastases should not undergo routine surveillance with brain magnetic resonance imaging (MRI). (Evidence quality = low.)
- Clinicians should have a low threshold for performing diagnostic brain MRI in patients with any neurologic symptoms suggestive of brain involvement, such as new-onset headaches, unexplained nausea/vomiting, or change in motor/sensory function. (Evidence quality = low, recommendation strength = strong.) ■
Disclosure: For complete disclosures of the guideline authors, visit jco.ascopubs.org.
References
1. Ramakrishna N, Temin S, Chandarlapaty S, et al: Recommendations on disease management for patients with advanced human epidermal growth factor receptor 2–positive breast cancer and brain metastases: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. May 5, 2014 (early release online).
2. Giordano SH, Temin S, Kirshner JJ, et al: Systemic therapy for patients with advanced human epidermal growth factor receptor 2–positive breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. May 5, 2014 (early release online).