In a phase III trial (CheckMate 037) reported in The Lancet Oncology, Jeffrey S. Weber, MD, PhD, of the Moffitt Cancer Center, and colleagues found that treatment with the PD-1 (programmed cell death protein 1) inhibitor nivolumab (Opdivo) resulted in a significantly greater response rate vs chemotherapy as second- or later-line treatment in patients with advanced melanoma progressing after anti–CTLA-4 (cytotoxic T-lymphocyte–associated protein 4) treatment.1 Findings in this trial supported the accelerated approval of nivolumab in this setting in December 2014.
Study Details
In this open-label trial, 405 patients with unresectable or metastatic melanoma from 90 sites in 14 countries were randomized 2:1 between December 2010 and January 2014 to receive nivolumab (n = 272) or chemotherapy (n = 133). Patients had to have progressed after treatment with ipilimumab (Yervoy) or with ipilimumab and a BRAF inhibitor if they were BRAF V600 mutation-positive.
Nivolumab was given at 3 mg/kg IV every 2 weeks. Dose delay but not reduction was permitted in nivolumab patients. Investigator’s choice of chemotherapy consisted of dacarbazine 1,000 mg/m2 every 3 weeks or paclitaxel 175 mg/m2 combined with carboplatin area under the curve = 6 every 3 weeks. Treatment was continued until disease progression or unacceptable toxicity. The primary endpoints of the trial were objective response and overall survival. In the current report of the first interim analysis, objective response was assessed after 120 patients had been treated with nivolumab and had a minimum follow-up of 24 weeks.
Among all randomized patients, the nivolumab and chemotherapy groups were generally balanced for age (median 59 and 62 years), sex (65% and 64% male), Eastern Cooperative Oncology Group performance status, stage M1c disease, stage 4 disease, history of brain metastases, elevated LDH, number of prior systemic treatments, previous treatment other than ipilimumab, PD-L1 (programmed death-ligand 1)–positive status, BRAF-mutant disease, and no benefit from prior ipilimumab.
Objective Response Rate
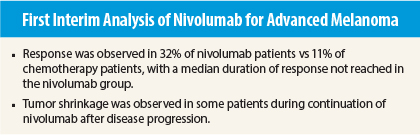
Patients received nivolumab for a median of 5.3 months and chemotherapy for a median of 2.0 months. Confirmed objective response was observed in 38 (31.7%, 95% confidence interval [CI] = 23.5%–40.8%) of the first 120 patients in the nivolumab group (including complete response in 4 patients, 3.3%) vs 5 (10.6%, 95% CI = 3.5%–23.1%) of 47 patients in the chemotherapy group. Median duration of response had not been reached (range = 1.4+ to 10.0+ months) in the nivolumab group and was 3.5 months (range = 1.3+ to 3.5) in the chemotherapy group. Median time to response was 2.1 months (range = 1.6–7.4 months) vs 3.5 months (range = 2.1–6.1 months).
At the time of analysis, 33 of 38 nivolumab patients (87%) with response had continuing response without disease progression on treatment. Nivolumab was continued beyond disease progression in 37 patients (31%), with 10 (8%) exhibiting more than 30% reduction in the sum of the longest diameters of target lesions.
Predefined Subgroups
In exploratory subgroup analyses, a higher response rate was observed with nivolumab vs chemotherapy irrespective of BRAF-mutation status or previous anti–CTLA-4 treatment benefit. Response was observed in 23.1% (6/26) vs 9.1% (1/11) of BRAF V600 mutation–positive patients and 34.0% (32/94) vs 11.1% (4/36) of BRAF–wild-type patients. Response was observed in 30.0% (12/40) vs 13.3% (2/15) of patients with prior anti–CTLA-4 treatment benefit and in 32.5% (26/80) vs 9.4% (3/32) with no benefit. Response was observed in 43.6% (24/55) vs 9.1% (2/22) of patients with PD-L1–positive tumors and in 20.3% (13/64) vs 13.0% (3/23) of those with PD-L1–negative tumors.
At the time of the first planned assessment of objective response, 182 patients had been randomized. Among these 182 patients, median progression-free survival was 4.7 months (95% CI = 2.3–6.5 months) vs 4.2 months (95% CI = 2.1–6.3 months; hazard ratio = 0.82, 99.99% CI = 0.32–2.05), and 6-month progression-free survival was 48% (95% CI = 38%–56%) vs 34% (95% CI = 18%–51%).
Adverse Events
The reported safety analysis included 268 nivolumab patients and 102 chemotherapy patients who received at least one dose of study treatment at the time of objective response analysis. The most frequent treatment-related adverse events of any grade in the nivolumab group were fatigue (25% vs 34% in the chemotherapy group), pruritus (16% vs 2%), and diarrhea (11% vs 15%); the most frequent adverse events in the chemotherapy group were nausea (37%), fatigue, and alopecia (27%).
Grade 3 or 4 treatment-related adverse events occurred in 9% vs 31% of patients, with the most common in the nivolumab group being increased lipase (1%), elevated alanine transaminase (1%), fatigue (1%), and anemia (1%). The most common grade 3 or 4 treatment-related adverse events in the chemotherapy group were neutropenia (14%), thrombocytopenia (6%), and anemia (5%).
Treatment-related serious adverse events occurred in 5% vs 9% of patients. Adverse events led to discontinuation of treatment in 3% vs 7%. No treatment-related deaths were observed.
The investigators concluded:
Nivolumab led to a greater proportion of patients achieving an objective response and fewer toxic effects than with alternative available chemotherapy regimens for patients with advanced melanoma that have progressed after ipilimumab or ipilimumab and a BRAF inhibitor. Nivolumab represents a new treatment option with clinically meaningful durable objective responses in a population of high unmet need. ■
Disclosure: The study was funded by Bristol-Myers Squibb. For full disclosures of the study authors, visit www.thelancet.com.
Reference
1. Weber JS, D’Angelo SP, Minor D, et al: Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol 16:375-384, 2015.
Kim A. Margolin, MD, of Stanford University Medical Center, offers her perspective on the promise of immune checkpoint inhibition.