Over the past decade, the use of peripheral blood stem cells has increased, and now about 75% of unrelated living donor transplants are performed using peripheral blood stem cells without supportive data in the unrelated donor setting. This trend is called into question by results of a large phase III randomized multicenter trial showing similar outcomes of transplant procedures with bone marrow and peripheral blood stem cells from unrelated donors. Although use of peripheral blood stem cells resulted in better engraftment, the rates of chronic and more extensive graft-vs-host disease were higher.
Rethinking the Shift in Stem Cell Sources
 “We need to rethink whether the shift to using peripheral blood stem cells over the past 10 years is justified. Both stem cell sources are acceptable. Peripheral blood stem cells may be preferred for patients at risk for graft failure, and bone marrow considered for all others. Research should be directed toward improving rates of graft-vs-host disease with peripheral blood stem cells and improving rates of graft failure with bone marrow,” said lead author Claudio Anasetti, MD, Chair of the Department of Blood & Marrow Transplant at Moffitt Cancer Center in Tampa, Florida. Dr. Anasetti presented the findings at a Plenary Session of the 53rd Annual Meeting of the American Society of Hematology in San Diego.1
“We need to rethink whether the shift to using peripheral blood stem cells over the past 10 years is justified. Both stem cell sources are acceptable. Peripheral blood stem cells may be preferred for patients at risk for graft failure, and bone marrow considered for all others. Research should be directed toward improving rates of graft-vs-host disease with peripheral blood stem cells and improving rates of graft failure with bone marrow,” said lead author Claudio Anasetti, MD, Chair of the Department of Blood & Marrow Transplant at Moffitt Cancer Center in Tampa, Florida. Dr. Anasetti presented the findings at a Plenary Session of the 53rd Annual Meeting of the American Society of Hematology in San Diego.1
Peripheral blood stem cells are currently being used by many centers in the United States as a source of adult stem cells because clinical trials of this strategy in related donors have shown lower relapse rates, better engraftment, and increased survival in patients with advanced leukemia and other blood diseases compared with the use of bone marrow stem cells. The present study prospectively analyzed outcomes with the two different stem cell sources in unrelated donors—and it appears to be the first study to compare them in this setting.
The open-label, prospective, comparative, multicenter study randomized patients from 50 transplant centers in the United States and Canada to receive bone marrow (n = 278) or peripheral blood stem cells (n = 273) as the graft source for transplant. The primary endpoint was 2-year survival on an intent-to-treat analysis. Both arms were well balanced for demographic and disease characteristics. Donor characteristics were also similar in both arms of the study. A variety of conditioning regimens were allowed. About 5% of those in the bone marrow arm and 4% in the peripheral blood arm did not undergo transplant.
Intent-to-treat Analysis
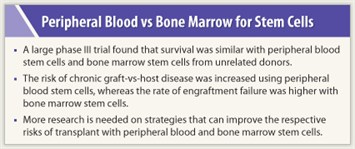 In the intent-to-treat analysis of all randomized patients, no difference in 2-year overall survival was seen between the two groups: 51% for peripheral blood stem cells vs 46% for bone marrow. The remaining analyses were restricted to patients who did undergo transplant. For this group, overall and disease-free survival were also not significantly different at 2 years. No interaction was found between survival and disease risk, donor HLA matching, or age.
In the intent-to-treat analysis of all randomized patients, no difference in 2-year overall survival was seen between the two groups: 51% for peripheral blood stem cells vs 46% for bone marrow. The remaining analyses were restricted to patients who did undergo transplant. For this group, overall and disease-free survival were also not significantly different at 2 years. No interaction was found between survival and disease risk, donor HLA matching, or age.
Primary graft failure was reported in 6% of bone marrow recipients and 1% of peripheral blood stem cell recipients; secondary graft failure occurred in 3% and 1%, respectively. Total graft failure rate was 9.1% in the bone marrow arm vs 2.7% in the peripheral blood arm, a significant difference favoring peripheral blood stem cells (P = .002). The incidence of acute graft-vs-host diseasewas similar between the two treatment arms, but the rate of chronic graft-vs-host disease was significantly higher in the peripheral blood arm: 32% for bone marrow vs 48% for peripheral blood stem cells (P = .01).
Of patients who were transplanted, more patients were alive and off immunosuppression in the bone marrow arm (57%) than in the peripheral blood stem cell arm (32%).
“Our trial demonstrates that when peripheral blood stem cells originate from unrelated donors, they are not superior to bone marrow stem cells in terms of patient survival, and they increase the risk of chronic graft-vs-host disease,” Dr. Anasetti stated. ■
Disclosure: Dr. Anasetti reported no potential conflicts of interest.
Expert Point of View: Which Is Better: Peripheral Blood or Bone Marrow as Unrelated Donor Stem Cell Source?
Reference
1. Anasetti C, Logan BR, Lee SJ, et al: Increased incidence of chronic graft-versus-host disease (GVHD) and no survival advantage with figrastim-mobilized peripheral blood stem cells (PBSC) compared to bone marrow (BM) transplants from unrelated donors: Results of Blood and Bone Marrow Transplant Clinical Trials Network (BMT CTN) protocol 0201, a phase III prospective, randomized trial. 53rd Annual Meeting of the American Society of Hematology. Abstract 1. Presented December 11, 2011.

 This large randomized, controlled trial took a lot of time and extensive resources, and yet survival was the same between the two types of unrelated donor transplant sources, noted Stephanie J. Lee, MD, Professor of Medicine at Washington University and the Fred Hutchinson Cancer Center in Seattle. ...
This large randomized, controlled trial took a lot of time and extensive resources, and yet survival was the same between the two types of unrelated donor transplant sources, noted Stephanie J. Lee, MD, Professor of Medicine at Washington University and the Fred Hutchinson Cancer Center in Seattle. ...