In a randomized phase II trial reported in the Journal of Clinical Oncology, Robert J. Motzer, MD, of Memorial Sloan Kettering Cancer Center, New York, and colleagues found that the programmed cell death protein-1 (PD-1) immune checkpoint inhibitor antibody nivolumab (Opdivo) was associated with antitumor activity and manageable toxicity at three dose levels in patients with metastatic renal cell carcinoma who had previously received vascular endothelial growth factor (VEGF) inhibitor therapy.1 No dose-response effect in progression-free survival (the primary outcome measure) was observed.
Study Details
In the study, 168 patients with clear cell metastatic renal cell carcinoma previously treated with VEGF inhibitors from 39 sites in the United States, Canada, Finland, and Italy were randomly assigned between May 2011 and January 2012 to receive intravenous nivolumab at 0.3 mg/kg (n = 60), 2 mg/kg (n = 54), or 10 mg/kg (n = 54) once every 3 weeks. The primary objective was to evaluate dose-response relationship measured by progression-free survival.
Overall, patients had a median age of 61 years; 72% were male; Memorial Sloan Kettering Cancer Center risk group was favorable for 33%, intermediate for 42%, and poor for 25%; Karnofsky performance status was 70 or 80 in 46% and 90 or 100 in 54%; and 82% had at least two evaluable sites.
Sites of lesions included lungs in 74%, lymph nodes in 58%, liver in 28%, skin/soft tissue in 24%, and adrenals in 22%; 36% had received prior radiotherapy; 98% had received prior surgery; the number of prior systemic therapies in the metastatic setting was one for 30%, two for 37%, and more than two for 33%; and the number of prior systemic antiangiogenic therapies in the metastatic setting was one for 62%, two for 33%, and three for 5%.
The most common prior systemic therapies in the metastatic setting were sunitinib (74%), everolimus (Afinitor, 34%), pazopanib (Votrient, 27%), interleukin-2 (Proleukin, 23%), and sorafenib (Nexavar, 19%). Overall, 118 patients (70%) had received more than one prior systemic regimen. In total, 107 patients (64%) had quantifiable PD-ligand–1 (PD-L1).
Progression-Free Survival
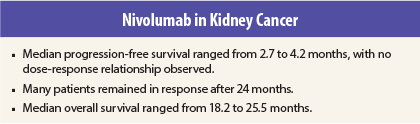
Median progression-free survival in the 0.3-, 2-, and 10-mg/kg groups was 2.7 months (80% confidence interval [CI] = 1.9–3.0 months), 4.0 months (80% CI = 2.8–4.2 months), and 4.2 months (80% CI = 2.8–5.5 months), respectively, with no dose-response relationship observed (P = .9 for trend). An exploratory analysis showed median immune-response progression-free survival of 4.3, 5.4, and 6.9 months (P = .6 for trend).
Response Rates
Objective response rates were 20%, 22%, and 20% (P = 1.0). Median time to response was 2.8 months (range, 1.3–5.6 months), 3.0 months (range, 1.4–6.9 months), and 2.8 months (range, 1.2–10 months). Median duration of response was not reached in the 0.3-mg/kg group and the 2-mg/ kg group and was 22.3 months in the
10-mg/kg group.
Among responders, 75% (9/12), 50% (6/12), and 45% (5/11) had ongoing response at the time of analysis. Overall, 40% (14/35) remained in response after 24 months and 7 were still in response that had not yet reached 24 months.
Overall Survival
Median overall survival was 18.2 months (80% CI = 16.2–24.0 months), 25.5 months (80% CI = 19.8–28.8 months), and 24.7 months (80% CI = 15.3–26.0 months). According to the authors, the median overall survival values were numerically higher than those reported in pivotal phase III trials in metastatic renal cell carcinoma.
Compared with the 0.3-mg/kg group, hazard ratios were 0.8 (80% CI = 0.6–1.1) in the 2-mg/kg group and 0.9 (80% CI = 0.6–1.2) in the 10-mg/kg group. Overall survival reflected Memorial Sloan Kettering risk group and was better in patients with one line of prior therapy than in those with more than one line.
Analysis by PD-L1 Expression
Exploratory analysis according to PD-L1 expression status showed that median progression-free survival was 4.9 months among patients with PD-L1 expression ≥ 5% (n = 29) and 2.9 months among those with expression < 5% (n = 78), response rates were 31% vs 18%, and median overall survival was not reached vs 18.2 months. Median progression-free and overall survival and response rate were similar between PD-L1–positive (n = 43) and PD-L1–negative (n = 64) patients when an expression cutoff of ≥ 1% for positivity was used.
Adverse Events
Treatment-related adverse events of any grade occurred in 75%, 67%, and 78% of patients in the 0.3-, 2-, and 10-mg/kg groups; the most common were fatigue (24%, 22%, and 35%), nausea (10%, 13%, and 13%), and pruritus (10%, 9%, and 11%). Overall skin-related adverse events occurred in 22%, 22%, and 28%. Hypersensitivity (all grade 1 or 2) occurred in 17% of patients in the 10-mg/kg group, compared with 2% of patients in each of the lower-dose groups.
Treatment-related grade 3 or 4 adverse events occurred in 5%, 17%, and 13% of patients, with no individual adverse event occurring in > 2% of patients in any group. No grade 3 or 4 pneumonitis was reported. Systemic corticosteroids were used for management of adverse events in 15%, 19%, and 33% of patients.
Treatment-related adverse events led to discontinuation of the study drug in 7%, 2%, and 7% of patients, with reasons including elevated serum aspartate transaminase level, cardiac disorder, endocrine disorder, nervous system disorder, and respiratory/thoracic disorder. There were no treatment-related deaths.
Based on findings in the current study and analyses of safety and efficacy across tumor types in a large phase I study, nivolumab at 3 mg/kg every 2 weeks has been selected as the monotherapy regimen to be used in further study.
The investigators concluded:
“Nivolumab demonstrated antitumor activity with a manageable safety profile across the three doses studied in [metastatic renal cell carcinoma]. No dose-response relationship was detected as measured by [progression-free survival]. These efficacy and safety results in [metastatic renal cell carcinoma] support study in the phase III setting.”
A phase III trial comparing nivolumab and everolimus in patients with metastatic renal cell carcinoma previously treated with antiangiogenic therapy and a phase III trial evaluating the combination of nivolumab and ipilimumab (Yervoy) in first-line treatment of metastatic renal cell carcinoma are underway. ■
Disclosure: The study was supported by Bristol-Myers Squibb and Ono Pharmaceutical Company. For full disclosures of the study authors, visit jco.ascopubs.org.
Reference