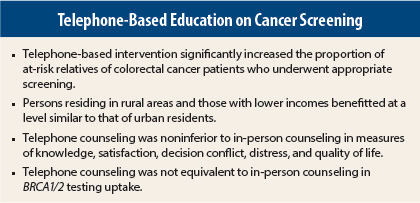
Two studies recently reported in the Journal of Clinical Oncology indicate that telephone-based education or counseling initiatives can be successful in educating individuals at familial or genetic risk of cancer and in inducing these at-risk individuals to undergo recommended screening.
In the Family CARE trial, Anita Y. Kinney, PhD, RN, Professor of Medicine at the University of New Mexico Cancer Center, Albuquerque, and colleagues found that a telephone-based strategy was effective in improving the colonoscopy screening rate in at-risk relatives of colorectal cancer patients.1 In another study, Marc D. Schwartz, PhD, Professor of Oncology at Georgetown Lombardi Comprehensive Cancer Center, Washington, DC, and colleagues found that telephone genetic counseling for BRCA1/2 mutation testing was noninferior to in-person counseling in the primary measures of knowledge, satisfaction, decision conflict, distress, and quality of life, but did not achieve equivalence with in-person counseling in test uptake.2
Intervention in At-Risk Relatives
In the Family CARE trial, 481 individuals aged 30 to 74 years who had not had risk-appropriate screening and were not candidates for genetic testing were recruited via contacting patients with colorectal cancer or their next of kin in five states (California, Colorado, Idaho, New Mexico, and Utah).1 Participants were randomly assigned as family units to receive active personalized intervention incorporating evidence-based risk communication and behavior change techniques (TeleCARE group, n = 232) or a mailed educational brochure (control group, n = 249).
All participants received a survey of self-reported baseline clinical information, including colonoscopy screening, family history of cancer, sociodemographics, and psychosocial data and a mailed educational brochure targeted to participant risk status. In addition, the TeleCARE group received mailed tailored visual aids, a tailored telephone cancer risk assessment and counseling session, mailed tailored summary letter of their telephone session, and a mailed tailored reminder card.
The TeleCARE intervention incorporated risk communication and behavior change approaches designed to improve perceptions about the threat of familial colorectal cancer, effectively manage fear, increase belief in colonoscopy benefits, and increase self-efficacy and motivation to undergo the procedure. Participants were informed that colonoscopy was the recommended screening strategy due to their risk status. Participants completed an outcome assessment at 9 months after the intervention. The primary outcome measure was verified colonoscopy within 9 months of the intervention.
The TeleCARE and control groups were generally balanced for age (mean, 50 and 51 years), race/ethnicity (white in 92% and 96%), marital status (74% and 77% married, 22% and 19%, separated, widowed, or divorced), educational level (43% post–high school in both, 22% and 27% Bachelor’s degree), residence (75% and 80% urban, 25% and 20% rural), household income (20% and 17% < $30,000, 18% and 20% $30,000–$49,999, 16% and 14% % 50,000–$69,999, 35% and 40% ≥ $70,000), employment status (72% and 69% employed), health insurance (private for 71% and 70%, no coverage for 16% and 20%), and proportion with a personal health-care provider (66% and 65%). Fewer TeleCARE group participants were female (39% and 46%).
Improved Colonoscopy Rate
Of all 481 at-risk relatives, 79.8% completed the outcome assessments within 9 months, with no significant difference between groups in retention rate. Overall, 35.4% of those in the TeleCARE group vs 15.7% of those in the control group underwent colonoscopy within 9 months (odds ratio = 2.83, P < .001). Odds ratios were similar and significant in subgroup analyses for rural residence (2.89, 95% confidence interval [CI] = 1.53–5.46), urban residence (2.87, 95% CI = 1.85–4.46), household income < $30,000 (2.75, 95% CI = 1.37–5.55), and household income ≥ $30,000 (2.94, 95% CI = 1.19–4.53).
The investigators concluded, “Remote personalized interventions that consider family history and incorporate evidence-based risk communication and behavior change strategies may promote risk-appropriate screening in close relatives of patients with [colorectal cancer].”
Genetic Counseling Strategy
In a noninferiority trial, 669 women aged 21 to 85 years with a minimum 10% risk for a BRCA1/2 mutation who did not have newly diagnosed or metastatic cancer were randomly assigned to telephone counseling (n = 335), in which all counseling was conducted by telephone, or usual care (n = 334), in which participants received in-person counseling before and after genetic testing for BRCA1/2 mutation.2 All participants were recruited from the clinical genetic counseling programs at Lombardi Comprehensive Cancer Center, Mount Sinai School of Medicine, University of Vermont Cancer Center, and Dana-Farber Cancer Institute.
Primary outcomes were noninferiority of telephone counseling in knowledge (Breast Cancer Genetic Counseling Knowledge Scale), satisfaction (Genetic Counseling Satisfaction Scale), decision conflict (10-item version of Decisional Conflict Scale), distress (cancer-specific stress with Impact of Event Scale, perceived stress with four-item version of Perceived Stress Scale), and quality of life (Short Form-12 Mental Component Summary and Physical Component Summary).
Secondary outcomes were equivalence of BRCA1/2 test uptake and costs of telephone counseling vs usual care. Interviews were conducted 2 weeks after counseling (pretest disclosure) and at 3, 6, and 12 months after randomization (post-test disclosure). The current report evaluated the 2-week and 3-month assessments.
The telephone group and the usual care group were balanced for age (mean, 48 years in both), BRCA1/2 probability (mean, 24% and 26%), education (at least college for 80% and 79%), employment status (full time for 59% and 55%), race (85% and 87% white), Jewish ethnicity (28% and 30%), being previously affected with breast or ovarian cancer (64% and 67%), proband status (63% and 64% probands), recruitment site (eg, Lombardi Cancer Center for 64% in both), and distance to the clinic (mean, 21 and 24 miles). BRCA1/2 testing was positive in 13% and 15%, negative in 17% in both, and uninformative/variant in 45% and 49%, with 25% and 19% remaining untested.
Noninferior Outcomes
Telephone counseling was noninferior to usual care on all primary outcome measures at 2 weeks: knowledge (difference [d] = 0.03, lower bound of 97.5% CI = −0.61), perceived stress (d = −0.12, upper bound of 97.5% CI = 0.21), and satisfaction (d = −0.16, lower bound of 97.5% CI = −0.70) had group differences and confidence intervals that did not cross the predefined 1-point noninferiority limit. Decision conflict (d = 1.1, upper bound of 97.5% CI = 3.3) and cancer distress (d = −1.6, upper bound of 97.5% CI = 0.27) did not cross the predefined 4-point noninferiority limit.
Sensitivity analyses confirmed noninferiority for all outcomes after adjusting for multiple comparisons and imputing for missing follow-up data. Results at the 3-month assessment were similar to those at 2 weeks.
Uptake Not Equivalent
Among the 600 women who completed pretest counseling (89.0% of the telephone group and 90.4% of the usual care group), 84.2% of the telephone group vs 90.1% of the usual care group underwent genetic testing (relative risk = 0.93, 95% CI = 0.88 to 0.99); the lower bound of the 90% CI (d = −5.9%, 90% CI = −10.3% to −0.01%) was outside the predetermined equivalence range, indicating that telephone counseling was not equivalent to in-person counseling. Similar results were found in the intention-to-treat population sample (74.9% vs 81.4%, d = −6.5%, 90% CI = −11.8% to 0.01%).
Cost Reduction
Telephone counseling reduced per-person cost by $114.40, with savings attributable to shorter counseling times, less patient travel, and lower overhead. On the assumption of identical overhead costs, savings were reduced to $59 per person. The greatest cost savings ($321.40 per person) was for use of in-home buccal DNA kits by rural participants.
The investigators noted that factors contributing to the lower testing rate in the telephone group may have included the fact that usual care participants were able to provide DNA immediately following counseling. While the delay between telephone counseling and DNA provision could be a barrier to testing, use of in-home buccal kits could increase test uptake.
The delay between counseling and DNA provision in the telephone group also allowed for greater deliberation that may have led some participants to forgo testing, a notion consistent with the fact that telephone counseling participants who declined testing had lower baseline risk scores and were less likely to consider risk-reducing surgery than those who completed testing.
The investigators concluded, “Genetic counseling can be effectively and efficiently delivered via telephone to increase access and decrease costs.” ■
Disclosure: The study by Kinney et al was supported by grants from the National Cancer Institute, Huntsman Cancer Foundation, and others. The study by Schwartz et al was supported by National Cancer Institute grants, Lombardi Comprehensive Cancer Center Biostatistics and Bioinformatics Shared Resource, and Jess and Mildred Fisher Center for Familial Cancer Research. For full disclosures of the study authors, visit jco.ascopubs.org.
References
1. Kinney AY, Boonyasiriwat W, Walters ST, et al: Telehealth personalized cancer risk communication to motivate colonoscopy in relatives of patients with colorectal cancer: The Family CARE randomized controlled trial. J Clin Oncol. January 21, 2014 (early release online).
2. Schwartz MD, Valdimarsdottir HB, Peshkin BN, et al: Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. J Clin Oncol. January 21, 2014 (early release online).