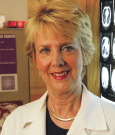
Nancy Kemeny, MD, Attending Physician at Memorial Sloan Kettering Cancer Center and Professor of Medicine at Weill Cornell Medical College, New York, discussed the study at the session and noted several limitations: The data could be outdated (chemotherapy and surgery could be better now), some patient- and treatment-related specifics were lacking or not reported, and the pathologic complete response rate of 6.8% is lower than most current reports (12%–28%).
However, she said that this large retrospective study “has given support to the concept” that a longer interval (more than 60 days) from the end of chemoradiation therapy to surgery is necessary to increase the chance of complete response, but waiting more than 60 days decreases overall survival.”
Discussing what is already known about rectal cancer treatment and outcomes, she pointed out that the attainment of a complete response is predictive of outcomes “and may allow for more tailored treatment.” For example, she indicated that many such patients are now avoiding surgery at Memorial Sloan Kettering, and results for this nonoperative management approach were reported at the Symposium.1 (These results were also reported in the February 10 issue of The ASCO Post. Visit ASCOPost.com to view them.)
Elaborating on the importance of achieving a complete response, she cited a study that assessed patients 6 weeks after neoadjuvant treatment and found that poor responders (by maximum standardized uptake values on PET/CT) were less likely to achieve a complete response (7% vs 38%) and less likely to demonstrate tumor regression (16% vs 45%).2
She added that large, bulky tumors need more time to achieve a complete response, but longer intervals may not be necessary for all tumors. “High” rectal tumors may need less time; however, “low” rectal tumors may need longer intervals when sphincter preservation is sought, she said.
Dr. Kemeny indicated that although it may take time to develop a complete response, in the absence of a tumor response, these longer intervals actually may be harmful. A longer wait time could facilitate local tumor growth and metastasis, enhance fibrosis, and delay the resumption of postoperative chemotherapy. ■
Disclosure: Dr. Kemeny reported no potential conflicts of interest.
References
1. Smith JJ, Chow OS, Eaton A, et al: Organ preservation in patients with rectal cancer with clinical complete response after neoadjuvant therapy. 2015 Gastrointestinal Cancers Symposium. Abstract 509. Presented January 17, 2015.
2. Perez RO, Habr-Gama A, São Julião GP, et al: Optimal timing for assessment of tumor response to neoadjuvant chemoradiation in patients with rectal cancer: Do all patients benefit from waiting longer than 6 weeks? Int J Radiat Oncol Biol Phys 84:1159-1165, 2012.