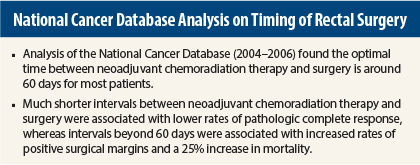
For the treatment of locally advanced rectal cancer, the optimal timing between the end of neoadjuvant chemoradiation therapy and surgical resection appears to be 60 days, according to an analysis of the National Cancer Database presented at the 2015 Gastrointestinal Cancers Symposium.1
An interval of 60 days or less was associated with a higher likelihood of pathologic complete response. A longer interval did not further increase response and, in fact, was associated with higher risks of positive margins and mortality, reported Jonathan C. Salo, MD, a surgical oncologist at the Levine Cancer Institute at Carolinas Medical Center, Charlotte, North Carolina.
“Several retrospective studies have shown that pathologic complete response rates increase with increasing radiation-surgery interval. Most retrospective studies have shown no difference in overall mortality with longer radiation-surgery interval, compared with a shorter interval, and some have even shown improved survival in patients who had a longer interval,” Dr. Salo said.
Dr. Salo and colleagues assessed patients in the National Cancer Database, which represents 70% of newly diagnosed cancer patients in the United States; contains 30 million records; and provides staging, treatment, and survival data. They examined data from 6,805 patients diagnosed with rectal adenocarcinoma between 2004 and 2006 and who underwent preoperative radiation therapy (most with chemotherapy), followed by radical surgical resection (excluding transanal excision). Surgery was done within 6 months of diagnosis and within 4 months of radiation therapy. The median follow-up for these patients was 5.6 years.
Pathologic Complete Response Optimized at 60 Days
“Increasing the radiation-surgery interval was associated with an increase in the rate of pathologic complete response up to 60 days (P = .0003), but the rate did not appear to increase thereafter,” Dr. Salo reported.
A longer radiation-surgery interval beyond 60 days was associated with an increase in the rate of positive surgical margins. Positive margin rates were 4.1% for an interval up to 30 days; 5.4% for an interval between 30 and 44 days; 4.8% for an interval between 45 and 59 days; 6.7% for an interval between 60 and 74 days; and 7.7% for an interval more than 75 days (P = .0067).
An interval beyond 60 days was also associated with shorter overall survival. When stratified by intervals of up to 60 days vs more than 60 days, the longer interval was associated with a 25% increased mortality risk, which was highly significant (P < .0001), he reported.
Dr. Salo proposed two explanations for the relationship between longer radiation-surgery interval and worse overall survival. It is possible, he said, that an increasing interval directly affects cancer outcomes, possibly through tumor regrowth, as suggested by the increase in positive margins shown in his study.
Other Prognostic Factors
Patients with longer intervals in the database may also have been affected by other factors, such as comorbidities, poor access to care, and older age, which can adversely affect cancer outcomes. Multivariate Cox modeling showed a number of factors associated with overall survival, including age (P < .0001), gender (P = .0034), insurance status (P = .0029), Charlson comorbidity score (P < .0001), tumor grade (P = .0004), clinical nodal status (P = .0006), pathologic tumor grade (P < .0001), pathologic nodal status (P < .0001), surgical margins (P < .0001), length of hospital stay (P < .0001), and radiation-surgery interval (P < .0001). On the other hand, the type of resection did not seem to affect long-term survival.
“Surgical margins were a highly powerful prognostic indicator, as was postoperative length of stay,” Dr. Salo noted. “Radiation dose, radiation boost, and elapsed radiation therapy time did not make a difference, but the interval between radiation therapy and surgery was important, even in the multivariate analysis, and was an important prognosticator for overall survival.”
The study found the delay between radiation therapy and surgery was longer for patients who were older; had more comorbidities; and were Hispanic, black, or uninsured. Longer intervals related to comorbidities or poor access to care could be related to worse survival but would not explain an increase in positive surgical margins with longer intervals, he suggested. He hypothesized that the interval between radiation therapy and surgery might directly be detrimental to overall survival, perhaps through regrowth of tumor. ■
Disclosure: Dr. Salo reported no potential conflicts of interest.
Reference
1. Huntington CR, Boselli D, Hill JS, Salo JC: Optimal timing of surgical resection after radiation therapy in locally advanced rectal adenocarcinoma: An analysis of the National Cancer Database. 2015 Gastrointestinal Cancers Symposium. Abstract 510. Presented January 17, 2015.