A focused update to the 2009 ASCO Clinical Practice Guideline Update on Chemotherapy for Stage IV Non-Small-Cell Lung Cancer reflects new evidence on maintenance therapy in patients with response or stable disease after four cycles of first-line cytotoxic chemotherapy.1 The 2009 update recommendation (recommendation A6) stated that cytotoxic chemotherapy should be stopped at progression or after four cycles in patients without response and evidence that did not support (1) continuation of cytotoxic chemotherapy until disease progression or (2) initiation of a different chemotherapy before disease progression in patients with stable disease or response to first-line therapy.2
New 2011 Recommendation
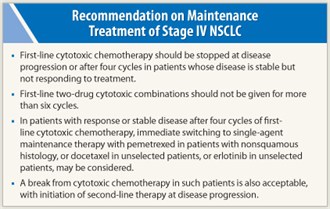 The 2011 focused update states that for patients with stable disease or response after four cycles, “immediate treatment with an alternative, single-agent chemotherapy such as pemetrexed in patients with nonsquamous histology, docetaxelin unselected patients, or erlotinib in unselected patients may be considered [italics added].” The recommendation also states that because of limitations of the data in this area, a break from cytotoxic chemotherapy in patients with response or stable disease after a fixed course of first-line therapy is also an acceptable option, with second-line treatment being delayed until disease progression.
The 2011 focused update states that for patients with stable disease or response after four cycles, “immediate treatment with an alternative, single-agent chemotherapy such as pemetrexed in patients with nonsquamous histology, docetaxelin unselected patients, or erlotinib in unselected patients may be considered [italics added].” The recommendation also states that because of limitations of the data in this area, a break from cytotoxic chemotherapy in patients with response or stable disease after a fixed course of first-line therapy is also an acceptable option, with second-line treatment being delayed until disease progression.
It continues to be recommended that first-line cytotoxic chemotherapy be stopped at disease progression or after four cycles in patients not responding and that two-drug cytotoxic combinations be given for no more than six cycles.
‘Switch Maintenance’ Trials
The focused update is based on review of data from seven phase III trials involving immediate non–cross-resistant alternative therapy (“switch maintenance”) in patients with response or stable disease after first-line treatment. The trials using docetaxel, pemetrexed (Alimta, in patients with non–squamous cell carcinoma), erlotinib (Tarceva), gefitinib (Iressa), and gemcitabine as switch maintenance therapy showed increased progression-free survival with maintenance therapy, with one of the two trials using erlotinib and the trial using pemetrexed also showing statistically significant increases in overall survival. These gains were accompanied by acceptable toxicity.
Key findings from these trials included the following:
- Immediate docetaxel showed an increase in progression-free survival vs delayed docetaxel (5.7 vs 2.7 months; P < .001) and a trend toward increased overall survival (12.3 vs 9.7 months; P = .0853).
- Pemetrexed showed prolonged progression-free survival (4.3 vs 2.6 months; HR = 0.502; P < .001) and overall survival (13.4 vs 10.6 months; HR = 0.79; P = .012) vs placebo, with benefit limited to patients with nonsquamous histology.
- Erlotinib significantly increased progression-free survival, though by only 1.2 weeks, vs placebo (12.2 vs 11.1 weeks; HR = 0.71; P < .001). Overall survival was prolonged by 1 month (12 vs 11 months; HR = 0.81; P = .0088).
In another trial, erlotinib or placebo was added to continued bevacizumab (Avastin) after four cycles of platinum-based therapy plus bevacizumab. Progression-free survival was prolonged for erlotinib vs placebo (4.8 vs 3.7 months; HR = 0.72; P = .0012), with no difference in overall survival.
The update committee did not specify erlotinib plus bevacizumab as an acceptable switch maintenance regimen because of lack of data showing an overall survival benefit of either maintenance bevacizumab alone or switch maintenance with erlotinib plus bevacizumab. - No benefit of carboxyaminoimidazole vs placebo was found after 3 to 6 months of chemotherapy in a trial closed due to slow accrual.
- Gefitinib vs continued platinum doublet chemotherapy (up to six cycles) produced a statistically but not clinically significant prolongation in progression-free survival (4.6 vs 4.3 months; HR = 0.68; P < .001), with no difference in overall survival.
- Progression-free survival was prolonged with maintenance gemcitabine (3.8 vs 1.9 months; HR = 0.55; P < .001) and maintenance erlotinib (2.9 vs 1.9 months; HR = 0.82; P = .002) vs observation after four cycles of cisplatin/gemcitabine, with no difference in overall survival based on preliminary findings.
ASCO guidelines indicate that patients with radiologic response after four cycles of first-line cytotoxic chemotherapy may be considered for continuation of treatment for two additional cycles. In line with this recommendation are data on switch maintenance therapy indicating better response with the cytotoxic agents docetaxel and gemcitabine in patients with response vs stable disease after four cycles of platinum-based first-line treatment.
Toxicity and Chemotherapy Breaks
The ASCO panel notes that the clinical trial data used for establishing the guidelines for duration of first-line chemotherapy involve drugs that are associated with cumulative toxicity and that the advent of new drugs without cumulative toxicity, as well as biomarkers for their effectiveness, will “complicate and perhaps diminish the importance of the question of optimal duration of therapy.”
The panel also notes that it would be of interest to analyze why some of the patients in the control arms of the reviewed studies, whose treatment had resulted in disease control after four cycles of first-line treatment, did not receive second-line treatment. In this regard, the panel states, “Until the time of further [overall survival] benefit shown in studies in which there was sufficient second-line therapy offered to participants in the control arm, and given the limitations of current data, the panel accepts as viable the traditional approach of allowing patients a break from cytotoxic chemotherapy after a fixed course of first-line therapy, with initiation of second-line chemotherapy at disease progression.”
Further Considerations
Important considerations in implementing the focused update include the following:
- The recommendation regarding switch maintenance generally applies to patients whose fitness is sufficient to tolerate increased adverse events.
- The recommendation for pemetrexed does not apply to patients receiving this agent as part of initial treatment, since such patients were not included in the study supporting the recommendation.
- Data are insufficient to suggest a best switch maintenance approach in patients receiving bevacizumab or cetuximab in first-line treatment, since such patients were not included in any trial showing OS benefit.
- There are no data to guide selection of best treatment for patents still responding to and tolerating platinum-based treatment after 4 cycles. In these patients, the traditional approach has been to continue first-line therapy, since there are data showing that delivery of cycles 5 and 6 improves PFS.
- The focused update recommendation involves only single-agentmaintenance therapy. Further, it does not specifically recommend for or against switch maintenance in patients with response or stable disease after 4 cycles of first-line therapy, with the option of second-line treatment delayed until disease progression. ■
SIDEBAR: The March of Progress in Lung Cancer Treatment
References
1. Azzoli CG, Temin S, Aliff T, et al: 2011 focused update of 2009 American Society of Clinical Oncology clinical practice guideline update on chemotherapy for stage IV non–small-cell lung cancer. J Clin Oncol. September 6, 2011 (early release online).
2. Azzoli CG, Baker S Jr, Temin S, et al: American Society of Clinical Oncology clinical practice guideline update on chemotherapy for stage IV non–small-cell lung cancer. J Clin Oncol 27:6251-6266, 2009.

 Before the discovery of predictive molecular tests (eg, EGFR mutation and ALK rearrangement), each chemotherapy drug for stage IV non–small cell lung cancer had about the same chance of success. Progress was made as more drugs were discovered. Patients lived longer with second- and third-line...
Before the discovery of predictive molecular tests (eg, EGFR mutation and ALK rearrangement), each chemotherapy drug for stage IV non–small cell lung cancer had about the same chance of success. Progress was made as more drugs were discovered. Patients lived longer with second- and third-line...